Background:
Our hospitalist group designs and delivers the inpatient lecture series for our residency program and we strive to ensure the topics are applicable to inpatient medicine. This non‐clinical responsibility is an increasingly common situation for academic hospitalists. In fact, almost a quarter of all full‐time hospitalist are involved in direct teaching and about 15% of hospitalists’ time is devoted to teaching.8 This evolution is supported by the learners who report increased satisfaction with educational value of rotations lead by hospitalists.3,4,6,7 Theoretically, billing data should accurately reflect the daily clinical work of hospitalists and the clinical exposure their residents and learners are experiencing.
Purpose:
We set out to analyze our billing data in order to identify potential deficits in our inpatient resident didactic curriculum.
Description:
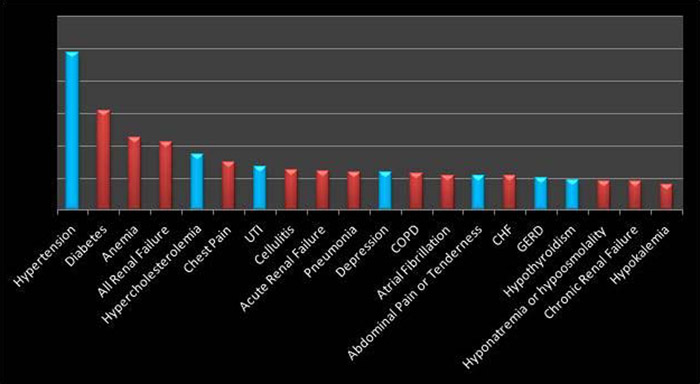
After the development and publication of the SHM Core Competencies, our hospitalist group adopted the Clinical Conditions as the framework for our inpatient lecture series. More recently, we questioned whether the content of this lecture series accurately reflects our case mix. We chose to answer this question through analysis of hospital billing data in order to identify potential deficits in the didactic curriculum. Two years worth of billing charges (Hospital Charges) were collected and analyzed. There were several pitfalls to this process, including the occasionally non‐clinical categorization of diagnosis related groups (DRGs). Overall, the process was not time consuming and is replicable for other academic hospitalist groups. The graphical results of our most commonly billed diagnoses are displayed in figure 1. Seven of our top twenty billed items were for diagnoses that are not covered in our current lecture series. Most of these diagnoses reflect chronic problems such as hypertension, hypercholesterolemia, depression, GERD and hyporthyroidism but acute issues were identified as well including urinary tract infection and abdominal pain.
Conclusions:
There have been other hospitalist academicians who have published regarding curriculum creation around identified deficits1 but there does not seem to be published information about the use of hospitalist billing data to inform inpatient curriculum to date. There is older data regarding curriculum development for family medicine residents based on outpatient exposures.2 We have created lectures for the acute illness items identified by our billing data that were not previously included in our lectures series and have begun to discuss the possibility of including more chronic disease teachings on the inpatient service. We have a particular interest in addressing depression since it has been identified as a major risk factor for readmission .5