Background: Given the convenience of placement and long term viability, PICC (peripherally inserted central catheter) utilization has been on a steady increase nationally over the last decade. Despite their advantages, PICCs are associated with minor complications such as dislodgement, luminal occlusion and superficial thrombophlebitis, and major complications including upper extremity thromboses and central line blood stream infections (CLABSIs). Many of these complications are correlated with PICC diameter and number of lumens. The recently released Michigan Appropriateness Guide for Intravascular Catheters (MAGIC) provides clinicians a framework to consider appropriateness of PICC use in various clinical scenarios.
Purpose: The goal of this project is to facilitate appropriate PICC utilization by implementation of a “PICC assessment tool” developed using the MAGIC criteria.
Description: The Michigan Hospital medicine and safety (HMS) consortium is a multi-hospital quality improvement initiative dedicated to preventing adverse events in hospitalized medical patients. Review of our hospital’s 2014 PICC utilization data from the consortium showed 59% of PICC lines were inserted for difficult venous access and blood draws and over 25 % PICCs were removed within 5 days of insertion.
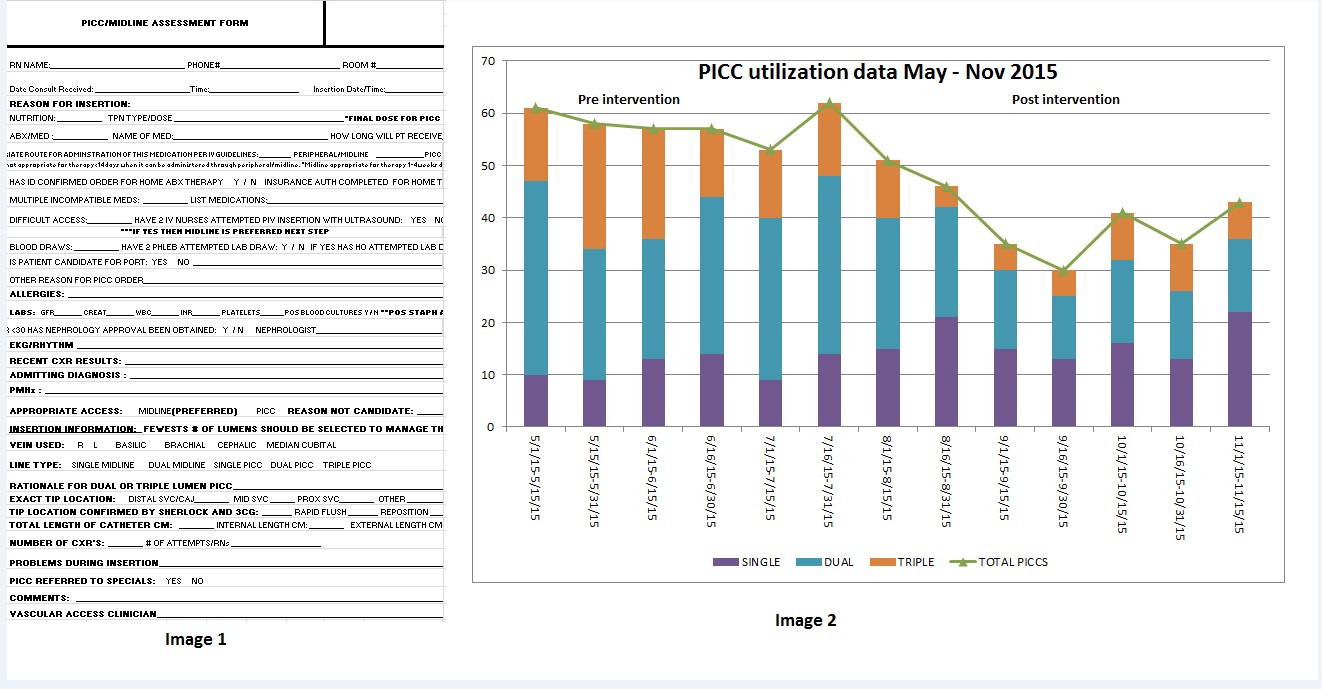
95% of PICCs at our institution are placed at the bedside by vascular access nursing. We developed a standardized assessment tool to evaluate the appropriateness of PICC request prior to placement (Image 1). The tool was designed by a multi-disciplinary team of physicians, vascular access nurses and pharmacy using the recently published MAGIC criteria. Beginning August 2015, vascular access nurses evaluated each PICC line request using the tool. Patients who did not meet the PICC appropriateness criteria had their vascular access orders changed to “midlines” or “US guided Peripheral IVs” after discussion with the ordering physician. Additionally, the vascular access team decided the appropriate number of lumens for each PICC placed based on clinical indications and discussions with pharmacy and other frontline providers. We also conducted multiple educational sessions to physicians, mid level providers and nurses on PICC related complications and stressed the importance of mindful PICC utilization.
Data was collected on overall PICC utilization and frequencies of single/double/triple lumen PICC and midline insertions. To evaluate the impact of the tool, we compared the PICC utilization data 12 weeks pre intervention (May-July 2015) to 14 weeks post intervention (Aug- Nov 15, 2015). Significantly fewer PICCs were inserted after implementation of the tool (348 pre-intervention vs 281 post intervention, P< 0.01). 40% of PICC requests were re-directed to other vascular devices after implementation of the screening tool compared to 24% prior to implementation. Additionally, we saw a significant decrease in triple lumen PICC utilization (18% vs 28%, P< 0.01) and a concomitant increase in single lumen PICC use (41 % vs 20 %, P< 0.01) (Image 2). Midline utilization also increased from 2% to 13% in the 3 months post intervention. Next steps involve studying the impact of decrease in utilization on PICC associated complications and evaluating roll out of the tool to other hospitals in our health system.
Conclusions: Use of a PICC appropriateness assessment tool is a potential strategy to decrease in appropriate PICC utilization and can be replicated by other institutions.