Background: Heart failure (HF) is one of the most common discharge diagnoses for Medicare beneficiaries. As part of the Affordable Care Act, the Center for Medicare and Medicaid Services initiated the Hospital Readmission Reduction Program which reduced payments to hospitals for excess readmissions for HF and other diseases. This quality improvement project focused not only on readmissions related to the general population of patients with decompensated HF, but more specifically on the relatively small number of HF patients who frequently access emergency healthcare, the HF High Utilizers. Our goal was to decrease the HF 30-day all-cause readmission rate at a large, urban academic hospital.
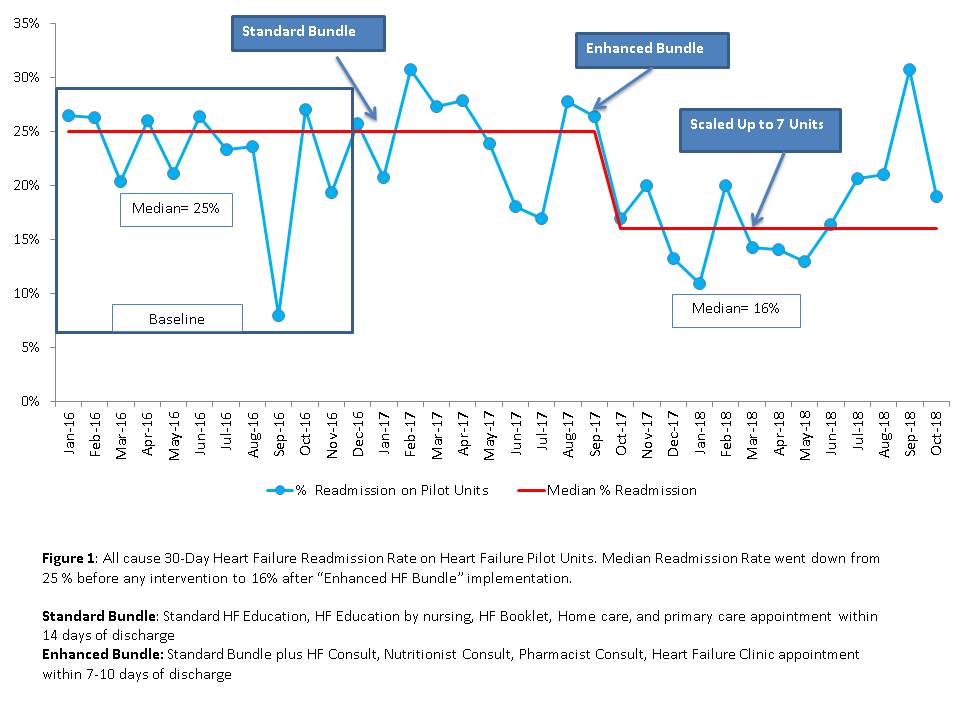
Methods: This project was conducted using standard quality improvement methodologies including Plan-Do-Study-Act cycles. As part of the initial phase of the project, decompensated Heart Failure patients were cohorted to four pilot units. All nursing staff on the pilot units were trained to deliver standard HF education. The initial intervention, performed in January 2017, was for all decompensated HF patients and included a “standard bundle” of HF education by nursing, HF Booklet, home care referral, and a primary care appointment within 14 days of discharge. Using additional QI tools, the team recognized that many of the readmissions were among HF High Utilizers, those patients with at least two HF index admissions and one HF related 30-day readmission in the previous 12 months. The next intervention, performed in September 2017, included focused decompensated HF and HF High Utilizers admitted for any cause. The “enhanced bundle” for HF High Utilizers included the standard bundle elements plus a mandatory HF Team consult, Nutrition consult, Pharmacy consult, scale distribution and a HF clinic appointment within 10 days of discharge. The project expanded to three additional units in March 2018. Run charts were used to plot the change in readmission rate over time and Wilcoxon Rank Sum testing was performed.
Results: There were a total of 84 patients who met the criteria for HF High Utilizers. The rate of effectively cohorting HF High Utilizer patients to pilot units increased from 40 % in August 2017 to 100% in September 2018. The HF 30-day readmission rate decreased from a median of 25% in 2016 to a median of 16 % in 2018 as evidenced by a shift on the run chart following the introduction of the enhanced bundle (Figure 1). This was statistically significant on Wilcoxon Rank Sum testing (p=0.002).
Conclusions: Our hospital demonstrated a statistically significant decrease in the all-cause 30- day readmission rate for HF from 25% to 16% using quality improvement methodologies, and focusing on HF High Utilizers and decompensated HF patients. This may represent an opportunity to target other smaller populations in order to reduce readmissions.