Background: As healthcare consolidation accelerates, healthcare systems must navigate logistical challenges in integration while continuing to provide high quality care to their patients. One area where this can be challenging is in a patient’s transition from one healthcare system to another; for example an inpatient transition to outpatient. This is a critical period as poor transitions can lead to higher readmission rates and poor patient outcomes. We share our experiences working in two actively merging large academic healthcare systems and utilizing a novel closed loop referral system between the separate electronic medical records (EMR) to improve the transition of patients from inpatient to outpatient.
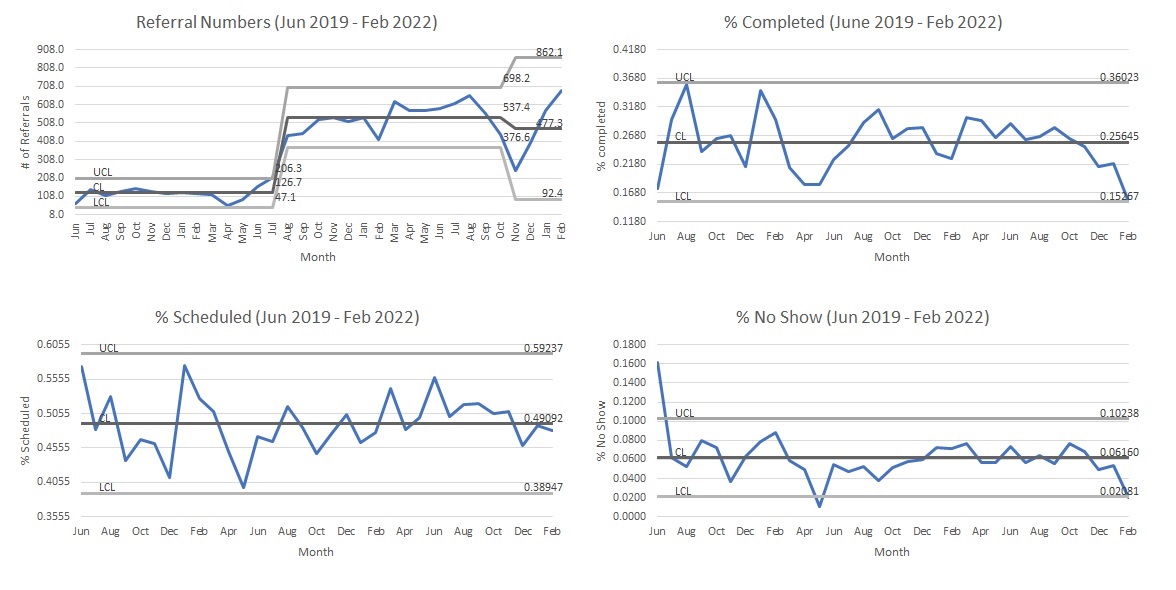
Methods: In 2014 our medical institution announced a joint venture with a local quaternary care hospital to develop a new hospital with work ongoing. Both institutions use the Epic EMR system but the systems are not integrated. Patients are frequently seen in the hospital and require outpatient care at a multi-specialty venture supported by the medical school. Prior to our interventions, there were only individual processes amongst the various subspecialists to schedule outpatient follow up. Most commonly patients were told to call to schedule their own appointments. No process provided a closed loop system, allowing for tracking of referrals or information between the two separate healthcare systems.Using end user feedback and input from a diverse group of stakeholders across both institutions, we developed a closed loop referral system that transmits referrals from the hospital to the outpatient providers. This system crosses two separate EMR systems by incorporating the Epic Care Everywhere Referral Management (CERM) system. After development of the new referral system, we actively engaged end users through educational videos, email reminders, and customized referral orders for specific subspecialty groups to facilitate their needs.Measures tracked including number of referrals placed, percentage of patients scheduled, and percentage of patient visits completed. We also tracked reasons patients were not scheduled.
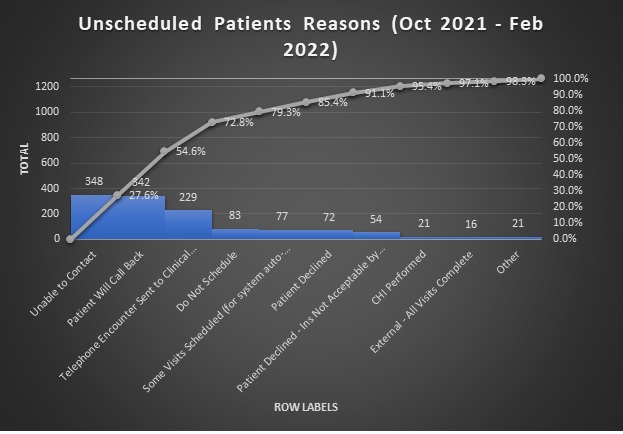
Results: The CERM system was implemented into the inpatient EMR system in June 2019. Extensive education was first given to the hospitalist group with eventual dissemination to all providers in the hospital. From June 2019 to February 2022, there were 11744 referral orders placed. Of those orders, 49% of the patients were scheduled but only 26% of orders resulted in a completed appointment. The most common reason for patients not being scheduled was due to inability to contact patients (27.6%). Challenges in coordination between IT departments and resources needed to maintain referral orders also led to breakdowns in the process and drops in referral orders. There was also significant variability in the time to available appointment for various subspecialties that contributed to poor outpatient follow up.
Conclusions: New intraoperability features in EMR’s like CERM offer merging healthcare systems mechanisms to bridge transitions to new processes and can be successful in promoting better healthcare practices. While CERM orders are a significant improvement over previous practice and ensure a transparent closed loop system, healthcare systems must also support ongoing collaboration between IT departments to prevent misfunctioning orders. There is also still much work to be done in improving patient capture rates with ability to contact patients being the ongoing challenge.