Background: Single-center studies have reported low yield of blood culture for skin and soft tissue infections (SSTIs) in children. Blood cultures are commonly obtained in cases of SSTI, though the degree of practice variation is uncertain. Study objectives include: 1) assess the degree of variation in rate of blood culture for SSTIs among children’s hospitals and 2) measure the rate of positivity of obtained cultures.
Methods: The Pediatric Hospital Information System (PHIS) Database was queried for years 2012-2017 for encounters grouped to All Patient Refined Diagnosis Related Groups (APR-DRG, 3M-HIS, Minneapolis, MN) 383, “ Cellulitis and Other Bacterial Skin Infections.” Index hospital encounters for children ages 2 mos-18 years were included if principal diagnoses contained International Classification of Diseases, version 9 (ICD-9) codes for erysipelas (035.x), cellulitis (680.x-682.x), impetigo (684.x), other localized skin infection (686.8-686.9), or super-infection (910-917.1, 910-917.3, 910-917.5, 910-917.7, 910-917.9), or matched ICD-10 codes. Patients were excluded if transferred from another facility, had history of immunodeficiency, malignancy or transplant, or had ICU care.Primary outcomes included rate of blood culture for SSTI encounters at each institution. Encounters with vs. without blood cultures were compared for length of stay (LOS), hospital costs and 30-day readmission rates. Outcomes were adjusted for demographics, number of complex chronic conditions (CCC) and severity of illness. Secondary outcomes included rate of positive blood culture, identified by ICD-9 codes for septicemia (038.x) or bacteremia (790.7) and matched ICD-10 codes.
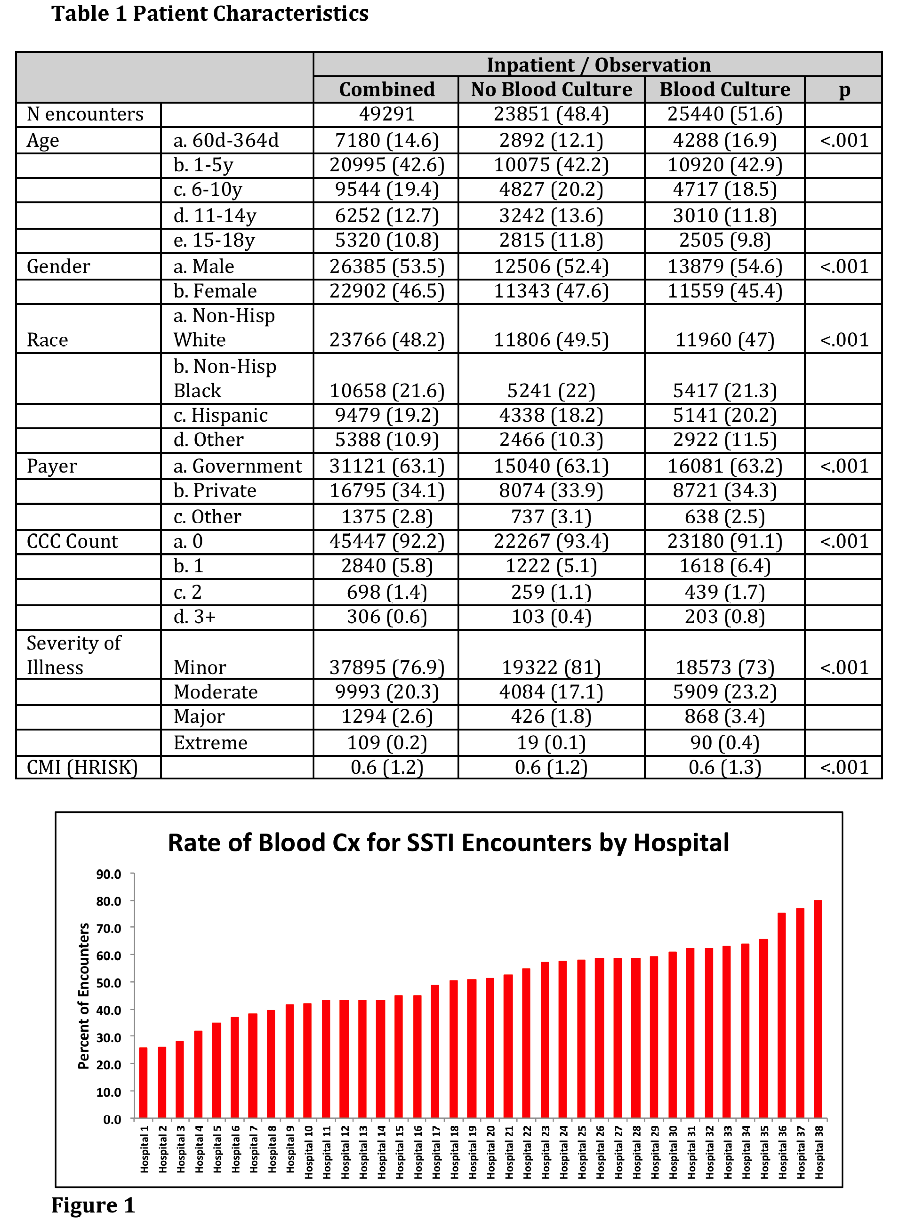
Results: We identified 49,291 hospital encounters for SSTI among 38 hospitals (Table 1). Overall, 51.6% of encounters had blood cultures, though rate varied substantially by hospital (25.4-79.9%, Figure 1).
In unadjusted analysis, encounters with vs. without blood culture had longer LOS (1.9 vs. 1.6 days, p<.001), higher hospital costs ($4030 vs. $3921, p<.001) and higher rate of readmission (1.3% vs. 1%, p=0.019). In adjusted analysis, encounters with vs. without blood culture had 20% longer LOS (RR 1.2, p<.001), 20% higher hospital costs (RR 1.2, p<.001) and 20% higher likelihood of readmission (RR 1.2, p=0.027).
The overall rate of bacteremia was 0.6%, though rate varied from 0.1-1.9%.
Conclusions: In our multi-center study of hospitalized children with SSTI, there was a high rate of blood culture with large variation across institutions. Encounters with vs. without blood culture had longer LOS, higher hospital costs and higher readmission rates. The rate of bacteremia was very low. Our data provide more evidence that blood cultures for children with SSTI are low-value practice.