Background: Acute otitis media (AOM) is a commonly overtreated pediatric diagnosis. Since 2014, the American Academy of Pediatrics (AAP) has recommended a ‘wait-and-see’ strategy and shorter antibiotic courses for mild or moderate AOM in qualifying patients. While this strategy has been successfully implemented in some pediatric emergency units (EUs), studies have shown that 30-90% of children with AOM treated in pediatric EUs do not get care consistent with these guidelines. We aimed to assess antibiotic prescribing practices in our tertiary care children’s hospital EU, calculate total possible cost savings of optimal management compared to current management, and stratify management by provider type to optimally direct future quality improvement efforts.
Methods: We performed a chart review of children >/= 2 diagnosed with AOM in the St. Louis Children’s Hospital (SLCH) EU. Inclusion criteria were age >/= 2 years, diagnosis of any form of “otitis,” and discharged between 5/1/2019 and 7/31/2020. Exclusion criteria were diagnosis of otitis externa, medical complexity, concurrent other bacterial illness, ear tubes, or recent antibiotic use. We analyzed this data using R v.3.5.2 software. Costs were estimated using price data from GoodRx™ and assuming a 20 kg child. Protocol was granted IRB exemption.
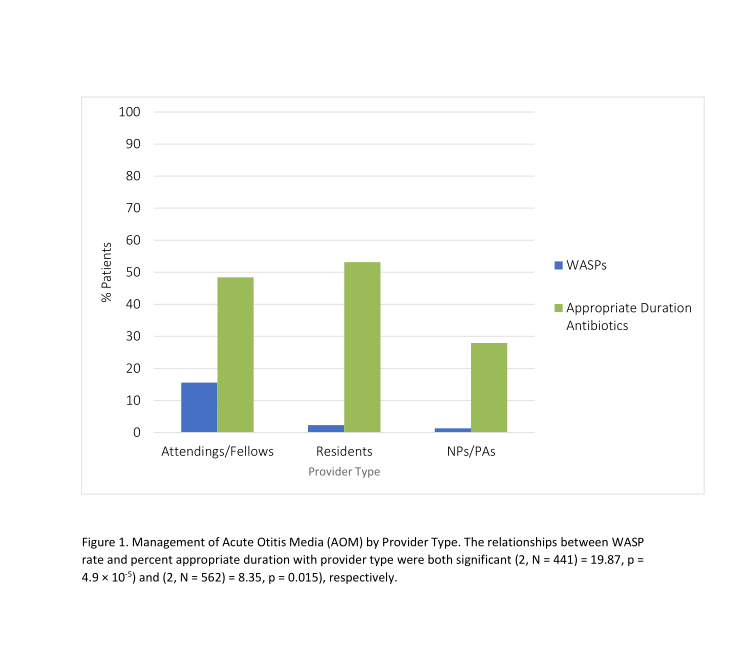
Results: 642 charts were reviewed and 570 were included in the analysis. Nurse practitioners (NPs) and physician assistants (PAs) discharged the majority of patients in our population (68%), followed by residents (20%) and fellows/attendings (12%). Severity was estimated using presence/height of fever, symptom duration, and presence of otorrhea/ear pain/bulging tympanic membrane. Of patients with likely non-severe AOM, 3% were prescribed WASPs. Stratifying by provider type, 15% of patients with likely non-severe AOM discharged by an attending/fellow were given WASPs, while only 2% of those discharged by residents and 1% by NPs/PAs were given WASPs. Taking into account severity and age, only 35% of patients who were prescribed antibiotics were prescribed an appropriate duration. For patients discharged with antibiotics by attendings or fellows, 48% were prescribed an appropriate duration, compared with 53% of patients discharged by residents and 28% of those discharged by an NP or PA. There was a significant relationship between provider type and management (p = 4.9e-5 for provider type/WASP, p = 0.015 for provider type/duration appropriateness by Chi-Square Test). Average cost savings per year were estimated at $4,804 for our patient population if optimal management strategies were implemented.
Conclusions: AOM management in our tertiary care children’s hospital EU is often not consistent with AAP guidelines. This is similar to results found by other recent studies of WASP use for pediatric AOM. We uniquely assessed rate of rates of WASPs and appropriate duration antibiotics between provider types, noting the potential for cost savings. Some variation was seen, but all provider types have substantial room for improvement. Possible barriers to appropriate AOM management include lack of knowledge of guidelines, established practice patterns, lack of time, or perception of parent desire for immediate antibiotics. To improve AOM management in our EU, our next steps will include implementation of a centralized guideline card, provider education, convenient ‘dot’ phrases to allow for more efficient documentation of counseling regarding WASPs in the electronic medical record, and continued tracking of data.