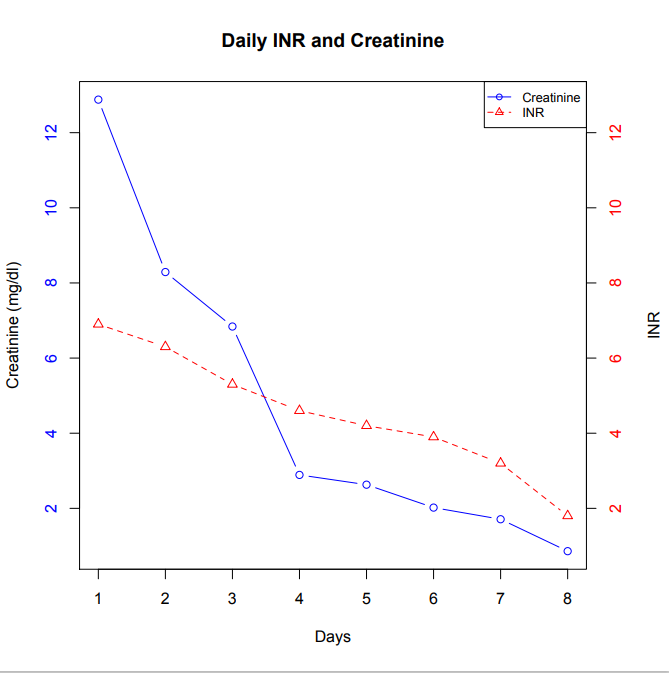
Case Presentation: 78yo male on chronic anticoagulation (warfarin) for pmh significant of three previous venous thrombosis (DVT), hypertension, diabetes, and hypercholesterolemia presented with one week of progressive right lower extremity erythema, edema, pain and tmax of 99F. On physical exam, he had tense, non-pitting edema and erythema from 10cm distal to the right knee to 5cm distal to the inguinal fold that was blanchable, warm and tender to palpation. No open lesions, skin breakdown, posterior calf or popliteal fossa tenderness. Labs significant for elevated WBC 15.5, creatinine 0.96 (baseline) and elevated INR of 6.6. Outpatient differential included lymphangitis, cellulitis, or DVT. Based on lab findings and physical exam, lymphangitis was declared as the primary diagnosis and he was treated with 1g IM Ceftriaxone followed by a 10 day course of sulfamethoxazole-trimethoprim 800-160mg and Cefadroxil 500mg.Two days after outpatient assessment, he was admitted to the hospital for worsening right lower extremity edema and erythema with suspected failed outpatient treatment. Labs on admission showed an (AKI) with serum creatinine of 12.88mg/dL, gross hematuria, dysmorphic RBC’s and significant proteinuria consistent with an acute glomerularnephritis. His Hg had dropped to 6.7 and his INR was supratherapeutic at 6.9. Bilateral lower extremity ultrasound showed acute DVT involving the right gastrocnemius and soleal veins.Further investigation for causes of his acute glomerular nephritis, supratherapeutic INR, AKI, and DTV included C3, C4, ANCA, thrombophilia panel + anticardiolipin IgG/IgM + beta 2 glycoprotein IgG/IgM, ANCA panel, ANA, CK, SPEP, free light chain kappa/lambda and PNH PI-Linked Antigen were all within normal limits. Based on aforementioned diagnostic findings and lack of alternative explanation for his AKI, gross hematuria and proteinuria, anticoagulation related nephropathy secondary to decreased renal function from outpatient antibiotic regimen, was declared as the cause.
Discussion: ARN is currently defined as acute kidney injury (AKI) without obvious etiology in the setting of an International Normalized Ratio (INR) of >3.0. In the few previously diagnosed cases of ARN, renal biopsies were done to confirm diagnosis. However given the risk of renal biopsies in the setting of an elevated INR, the diagnosis of ARN no longer relies on demonstration of these characteristic pathologic lesions. The underlying molecular mechanism is thought to be warfarin-induced thrombin depletion; however, newer studies have hinted at an alternative mechanism involving reductions in activated protein C and endothelial protein C receptor signaling. (1) Differences in the incidence and severity of ARN between patients taking warfarin and those taking novel oral anticoagulants are unknown; a post hoc analysis of routinely reported adverse renal outcomes in clinical trials comparing warfarin and novel oral anticoagulants found no significant difference in the rates of AKI, a prerequisite for ARN.
Conclusions: Treatment of ARN is supportive and includes returning the INR to a therapeutic range. There is no evidence that rapid reversal of INR limits kidney injury. The best approach to ARN is prevention and early detection. Anticoagulation levels and renal function should be monitored periodically. Lastly, as warfarin has a number of drug-drug interactions that can cause elevated INRs, close monitoring whenever new medications or other medical interventions are started, is essential.