Case Presentation:
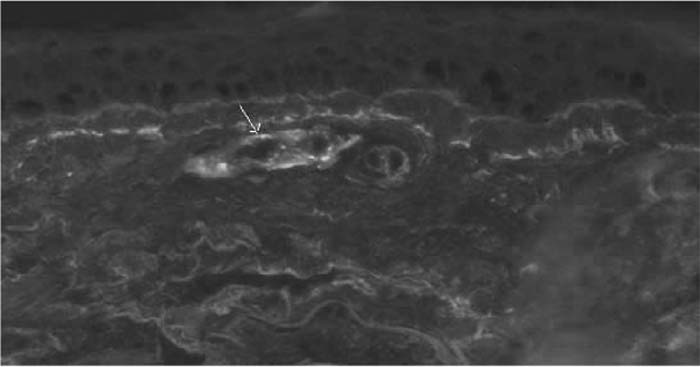
A 65‐year‐old Middle Eastern man with a history of coronary artery disease, chronic renal failure stage III, diabetes mellitus, and gout was admitted with hematuria and a purpuric rash on his upper and lower extremities. Bladder ultra‐sound revealed a bladder tumor, and cystoscopy with biopsy confirmed papillary urothelial neoplasm; hence, hematuria was presumed secondary to the bladder tumor. Urine analysis was negative for dysmorphic RBCs. A biopsy of his rash revealed leukocytoclastic vasculitis. He had recently been started on allopurinol, and because of its association with leukocytoclastic vasculitis, it was discontinued, resulting in partial improvement in the rash. However, the following week the rash recurred, with the development of acute on chronic renal failure. Further blood work revealed elevated serum immunoglobulin A (IgA) levels, normal C3 and C4 levels, a negative hepatitis panel, negative urine streptococcal antigen, and elevated inflammatory markers. Repeat biopsy of the skin with direct immunofluorescence (IF) antibody localization demonstrated perivascular deposits of complement C3, fibrinogen, and IgA (Figure 1), consistent with Henoch‐Schönlein purpura (HSP)
Figure 1. Immunofluorescence with anti‐lgA antibodies. IgA deposits are found in the walls of small superficial capillaries (white arrow).
Discussion:
HSP is usually seen in children but is very rare in adults. It is an immune‐mediated vasculitis of small vessels associated with IgA deposits. HSP in adults can present as a variable combination of palpable purpura, abdominal pain, arthritis, and renal disease. A retrospective analysis in adults with HSP has shown purpuric rash in nearly all patients and renal impairment in approximately a third of patients. Our patient had an unusual presentation with a waxing‐and‐waning purpuric rash involving all his extremities and renal impairment without any abdominal or arthritic symptoms. Diagnosis of HSP is based on clinical manifestations of the disease, but confirmation requires histopathological evidence of leukocytoclastic vasculitis with IgA deposits under IF in the affected organ. Although treatment with steroids and cyclophosphamide has been shown to benefit children with renal impairment, concrete evidence in adults is still lacking. Overall, adults with HSP tend to do poorly compared with children.
Conclusions:
HSP needs to be considered in adult patients with suspected cutaneous vasculitis, as it does not follow the typical clinical presentation seen in thepediatric population. HSP is an underdiagnosed condition in adults and appropriate early diagnosis hopefully might improve the clinical course and outcome
Author Disclosure:
S. Manda, none; A. Ramaswamy, none; M. Patel, none.