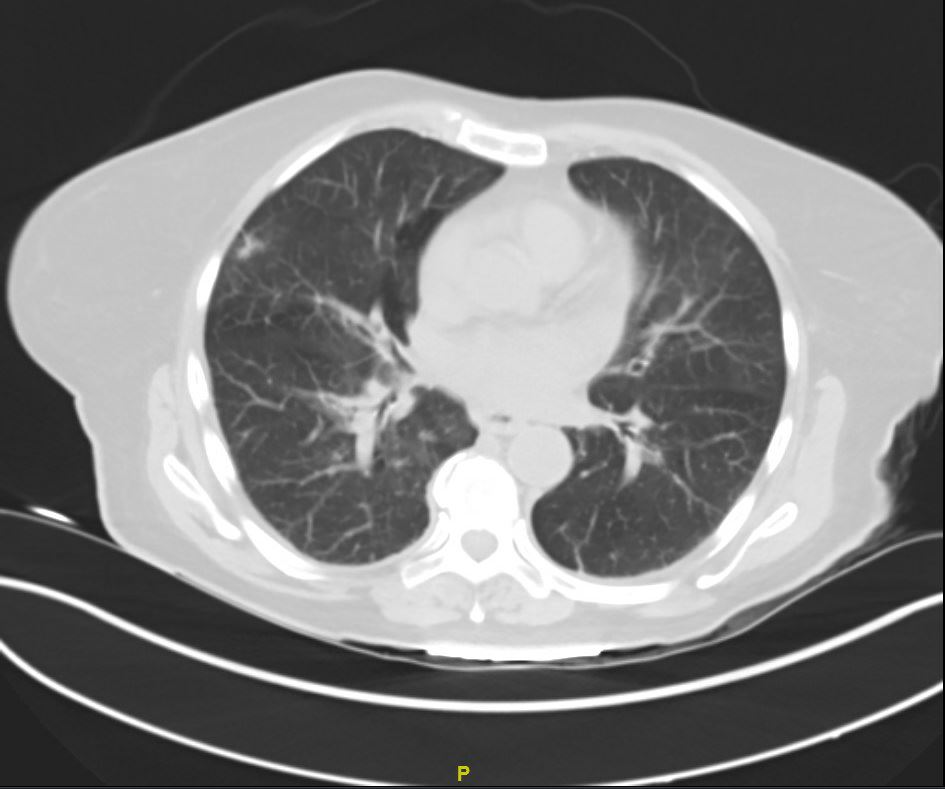
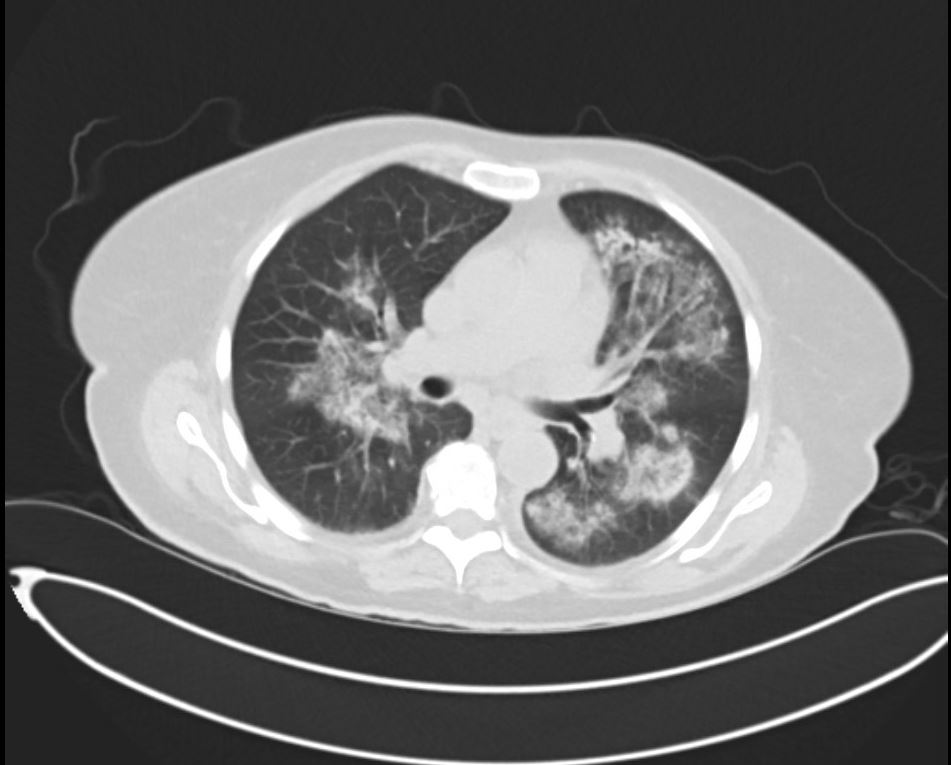
Case Presentation: A 60-year-old female with a history of diabetes and a recent diagnosis of COVID-19 four weeks ago presented to the hospital with a persistent cough, fatigue, and poor appetite. She had been discharged two weeks prior for chest pain and shortness of breath, felt to be secondary to COVID-19 induced myopericarditis. She was treated with colchicine and ibuprofen, although she only took the medications for a few days and then was told to stop by her primary care provider due to acute kidney injury. Her home medications also included lansoprazole and fluticasone. There is no family history of autoimmune disorders. Physical examination at the time of admission was only remarkable for conjunctival pallor. She was noted to have a temperature of 100.4 and hemoglobin of 6.5g/dl. Her CRP was 180 mg/L, and d dimer was 2,030 ng/ml. She maintained adequate oxygen saturation on ambient air. Iron studies revealed elevated ferritin and low iron. She received two units of packed red blood cells with improved hemoglobin up to 9.5g/dl. SARS-CoV2 test was negative. On day 3 of her hospitalization, her creatinine increased up to 2.96mg/dl from 2.65mg/dl at the time of admission. Her urine analysis revealed gross hematuria and proteinuria. Rheumatologic workup showed elevated c-ANCA titers (1:320) and elevated proteinase3 antibodies (>8.0 antibody index). Her protein creatinine ratio was 2.0, and microalbumin creatinine ratio was 636. CT scan of her chest revealed bilateral perihilar areas of dense lung consolidation.On day 4, her creatinine increased up to 3.22mg/dl. Nephrology and Rheumatology recommended starting intravenous solumedrol 500mg once daily for COVID-19 induced glomerulonephritis and presumptive Granulomatosis with polyangiitis (GPA). On day 5, her creatinine was 4.18 mg/dl. A renal biopsy was done that revealed severe crescenteric and necrotizing glomerulonephritis. She was started on rituximab with gradual improvement in her renal functions.
Discussion: GPA is a condition characterized by a necrotizing granulomatous vasculitis with the ability to affect different organs. Lung involvement has been reported in many cases; hence, a CT scan is commonly performed in GPA. Significant chest CT scan findings are ground glass opacities (GGOs), consolidation, septal thickening, and reticulations. These features are, nonspecific and can be seen in other conditions, including COVID-19 pneumonia and Pneumocystis carinii pneumonia. Lung hemorrhage, seen in the disease’s active phase, may present as GGOs and consolidation in CT studies. As GPA and COVID-19 pneumonia share clinical and radiological features, discrimination based on imaging can be challenging.COVID-19 patients also sometimes present with acute kidney injury and hematuria due to rhabdomyolysis. Clinicians are blind-sighted by COVID-19, often missing conditions such as GPA. Despite being in a pandemic, clinicians must think of other conditions that affect multiple organ systems, especially when the clinical picture is not consistent with COVID-19. Our patient had normal oxygen saturation and down-trending inflammatory markers, yet her renal function deteriorated with the presence of hematuria and proteinuria in her urine.
Conclusions: Early diagnosis of GPA can be difficult and requires a high index of suspicion in all patients, but especially in cases with atypical presentation. Prompt diagnosis and appropriate management of GPA in patients previously infected or co-infected with COVID-19 is essential to reduce morbidity and mortality.