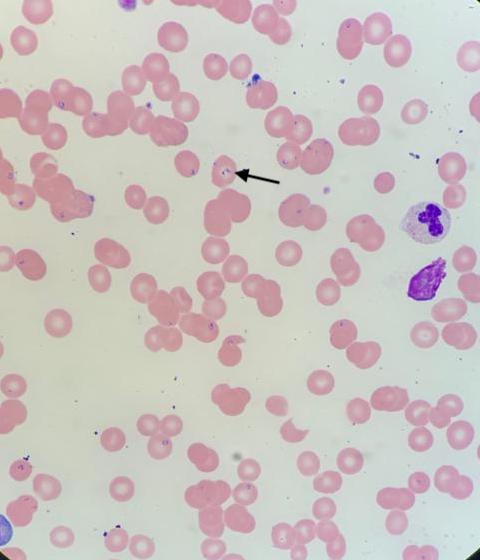
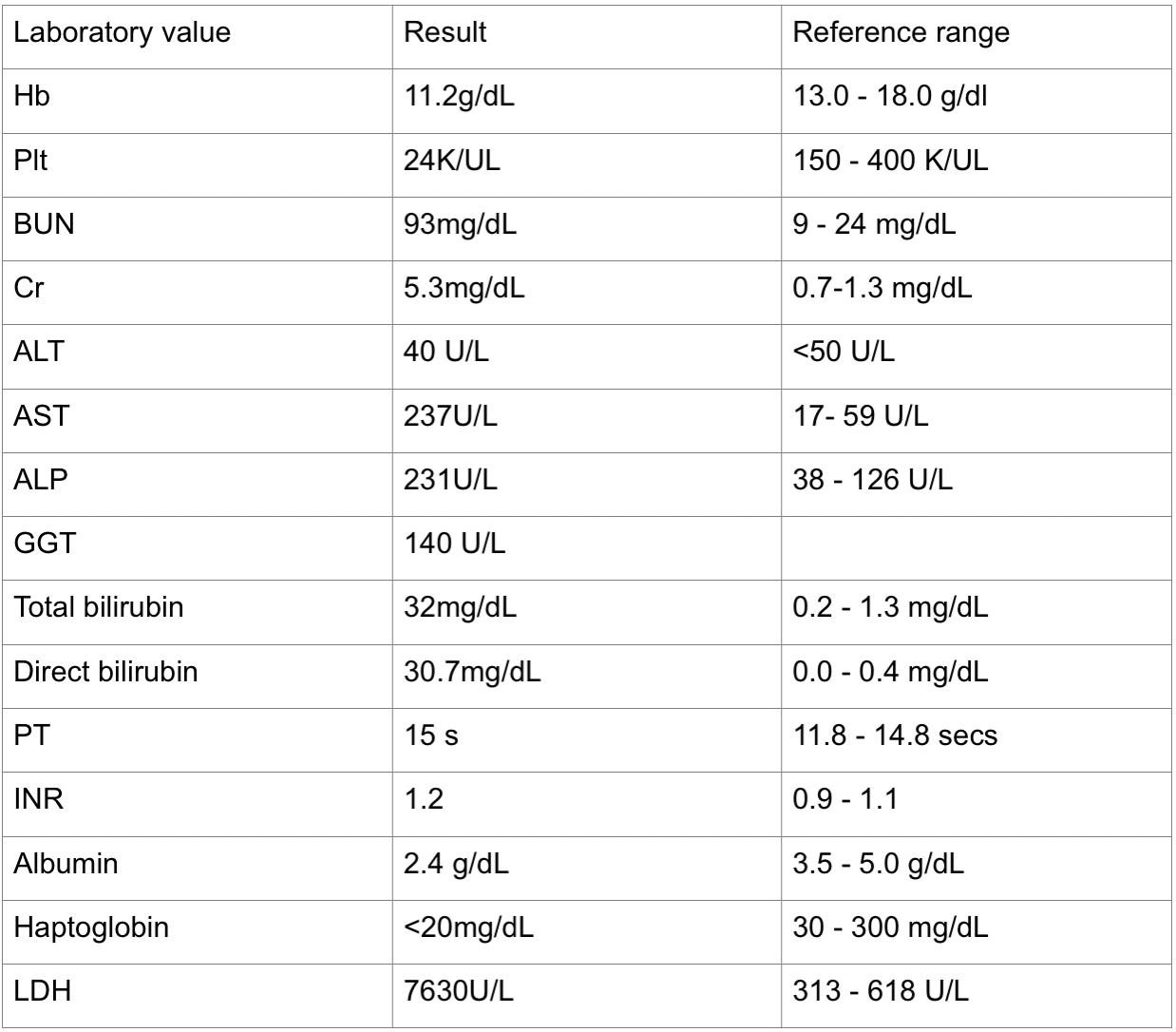
Case Presentation: A 44 year old man with a history of alcohol abuse presented with one week of right upper quadrant (RUQ) pain, nausea, jaundice, fevers, lethargy and anorexia in the summer time after two weeks of binge drinking. Physical examination was notable for tachycardia, scleral icterus and RUQ tenderness. Pertinent labs included elevated AST:ALT ratio of 5:1, direct hyperbilirubinemia (DH), anemia, thrombocytopenia and elevated creatinine (Table 1). Viral hepatitis panel was negative. RUQ US was negative for biliary obstruction. He was treated for acute alcoholic hepatitis and acute renal failure with concern for hepatorenal syndrome. One day later, he developed anuria and acute respiratory distress. He was started on bicarbonate infusion, corticosteroids and octreotide. Laboratory studies showed worsening anemia, reticulocytosis, elevated LDH and decreased haptoglobin. Peripheral smear showed schistocytes and intraerythrocytic ring shaped inclusions (Figure 1). Babesia was confirmed with a parasitemia load of 9.2%. He received IV clindamycin, doxycycline, quinine and one session of plasma exchange. He was also started on hemodialysis. Testing for HIV, Anaplasma and Lyme Disease were negative. His ICU course was complicated by ARDS, cardiac arrest, pneumonia and pancreatitis. He was successfully resuscitated, extubated and completed a course of culture directed antibiotics with a result of 0% parasitemia after 15 days. He developed a spontaneous intracerebral hemorrhage with midline shift; due to poor prognosis, patient had palliative extubation and expired.
Discussion: Babesiosis is a tick-borne infection caused by an intraerythrocytic protozoan which is endemic to the northeastern US, often with increased incidence in the summer (1,2). Patients may be asymptomatic or present with severe disease when accompanied by parasitemia >4%. Unlike our patient, those most at risk for severe presentations are >50 years and are immunocompromised (1,3). Concurrent alcohol use may be a contributing factor to the severity of disease (1).The pathophysiology of severe babesiosis is complex. The traditional model of babesiosis starts with red cell lysis and subsequent indirect hyperbilirubinemia, hemoglobinuria and renal impairment (4). Our patient had an unexpected finding of severe, isolated DH in the presence of hemolysis with negative biliary obstruction on ultrasound. Marked DH in patients with babesiosis has also been observed in some studies, but the pathogenesis remains unclear (5). Animal studies have shown intense hepatic parenchymal and perivascular inflammation as result of chronic babesiosis (5). Other hypothesized mechanisms for hepatic necrosis include direct injury from the organism, cytokine induced oxidative stress and hypoperfusion (3,6).
Conclusions: This case highlights the importance of having a high index of suspicion for severe babesiosis in patients who reside in endemic regions presenting with acute liver impairment along with laboratory signs of hemolysis, even when accompanied by a direct hyperbilirubinemia.