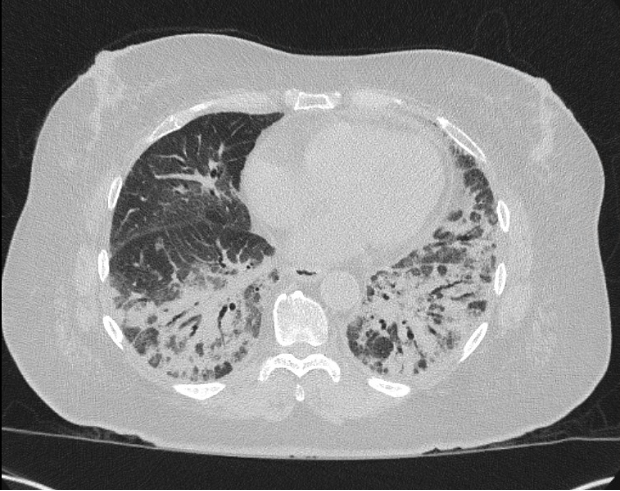
Case Presentation: A 75-year-old female with a medical history of type II diabetes mellitus, asthma, and arthritis presented with approximately three months of recurrent pneumonia. On admission, she complained of progressive generalized weakness with associated shoulder pain, shortness of breath, cough with foul-smelling sputum, and new, bilateral wrist swelling. Vital signs were significant for tachypnea and a fever (100.6 F). Initial complete blood count (CBC) was notable for anemia (Hgb 9.6, HCT 29.6) and leukocytosis to 12.2. Repeat CBC on day three of admission was significant for eosinophilia (eosinophil # 1.0, % eosinophil 6.6) with elevated c-reactive protein (CRP) to 101.9 and erythrocyte sedimentation rate (ESR) to 56. Chest X-ray showed likely multifocal pneumonia, and chest computed tomography (CT) scan showed worsening basilar predominant consolidation when compared to scans from a month prior when she was hospitalized for dyspnea (Figure 1). Given that she previously completed multiple courses of antibiotics (azithromycin, amoxicillin/clavulanate, levofloxacin, linezolid) and appeared clinically well, empiric antibiotics were held. Two days into her admission, she developed a diffuse, pruritic rash along her arms, legs, and buttocks that she attributed to recent use of antibiotics. A skin biopsy showed urticarial vasculitis. Infectious workup, including fungal and parasitic studies, were negative. Lung biopsy was consistent with an organizing pneumonia. Given these findings, there was concern for an underlying rheumatologic process that prompted consultation and extensive rheumatological workup. While the bulk of this workup was also negative, the myositis panel returned positive for PL-12 antibody. She was ultimately diagnosed with anti-synthetase syndrome. In close consultation with the pulmonology and rheumatology teams, the patient was pulse dosed with 1-gram solumedrol daily for three days. She was discharged on 60 mg prednisone for four weeks, with scheduled follow-up with pulmonology, rheumatology, and dermatology.
Discussion: Anti-synthetase syndrome (ASS) is a rare, autoimmune disorder characterized by a myriad of signs and symptoms including fever, myositis, arthritis, Raynaud’s phenomenon, “mechanic’s hands” and interstitial lung disease (ILD) (1-2). ASS is associated with anti-synthetase antibodies, of which eleven have been identified (1). While anti-Jo1 tends to be the most common detected autoantibody, anti-PL12 reportedly accounts for < 10% of cases (1-2). When comparing long-term outcomes between anti-Jo1 and anti-PL7/PL12 positive ASS, anti-PL7/PL12 positive ASS has been found to be strongly associated with severe and progressive ILD (2). Interestingly, urticarial vasculitis has not been reported as a cutaneous manifestation of ASS (3), and was likely a separate autoimmune process at play. In terms of treatment, corticosteroids have been the mainstay, however there is emerging evidence to support the efficacy of rituximab in the treatment of ASS (1).
Conclusions: Here we present a case of PL12 positive ASS that had been previously treated as recurrent pneumonia in both inpatient and outpatient settings. This case underscores the importance of having a keen eye and healthy level of suspicion in situations where standard treatment (in this case, antibiotics) is ineffective.