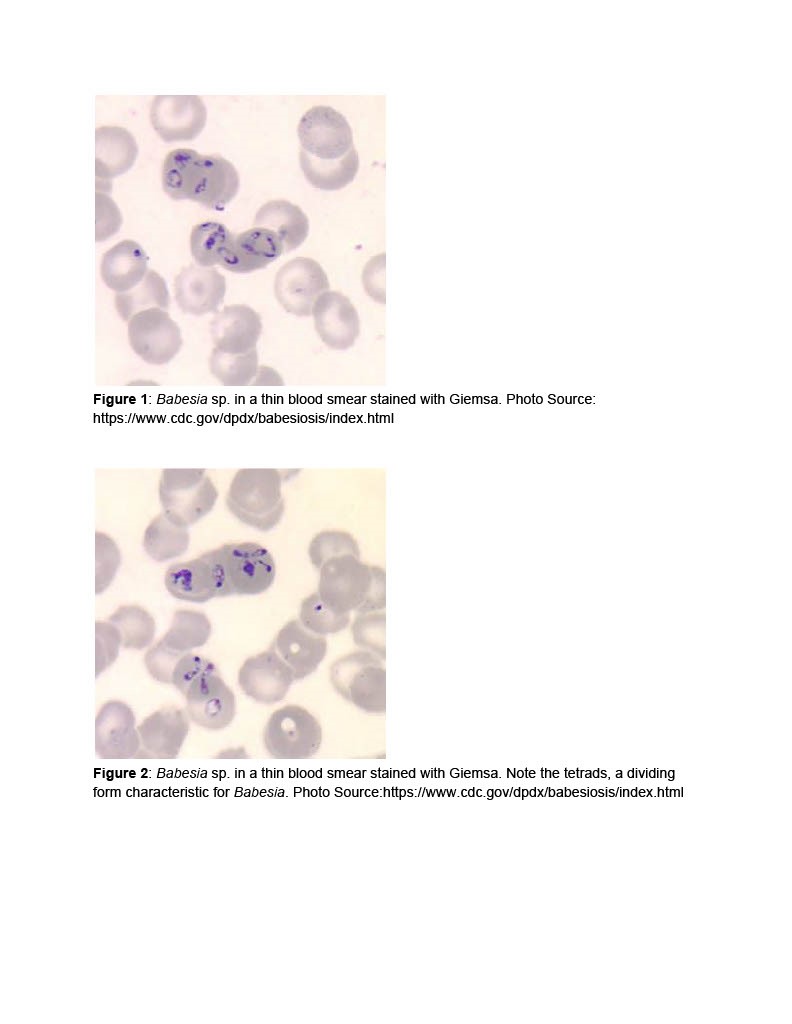
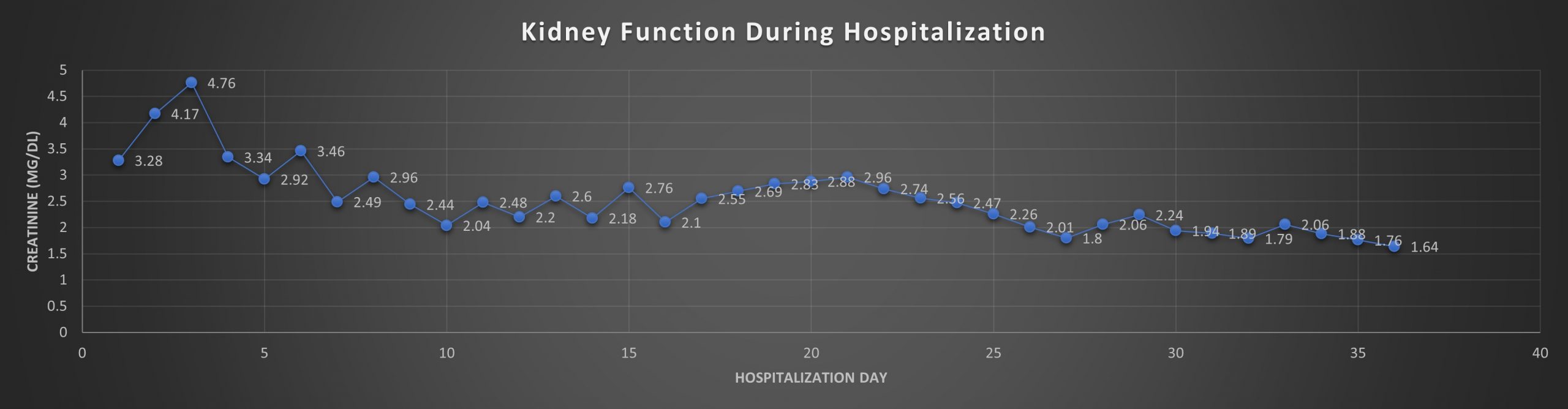
Case Presentation: 74-year-old female with history of heart failure, hypertension, diabetes, CKD Stage 3, obstructive sleep apnea, and COPD (2L O2 baseline) presented with weakness and shortness of breath for the last few days. She also endorsed having weight gain, despite a decrease in appetite. Apart from this, she reported a recent tick bite. On admission, she was hypoxic (requiring 4-5 L O2), labs showed thrombocytopenia, transaminitis, AKI, hyperbilirubinemia and peripheral blood smear showed inclusion bodies suggesting Babesiosis. She was admitted to ICU for decompensated CHF and severe Babesiosis with multi-organ dysfunction. Treatment with Atovaquone and Azithromycin was initiated. Urine microscopy showed muddy brown casts indicative of ATN; which along with uremic encephalopathy, necessitated dialysis, with modest improvement.In the following days, her mentation worsened, requiring a 2nd round of Azithromycin/Atovaquone. Consequently, her labs improved, however she developed status epilepticus, requiring intubation. For seizure management, she was started on Keppra.Unfortunately, she remained encephalopathic; MRI and LP were done and were noncontributory. It was concluded that her neurological symptoms were due to overwhelming sepsis secondary to Babesiosis. After a 3rd round of Azithromycin/Atovaquone, her mentation eventually improved, and she was discharged. On discharge, she was alert and oriented with improvement in creatinine to 1.64 mg/dl (3.28 mg/dl at presentation).
Discussion: The intraerythrocytic protozoan species Babesia microti is the most common cause of Babesiosis [1]. Mild to moderate disease, <4% parasite index, typically occurs in healthy individuals with symptoms developing within 1-4 weeks of tick bite [11]. Symptoms include fatigue, myalgia, fever, and weakness. Coinfection with Borrelia burgdorferi may occur, causing symptoms to persist longer. An elevated LDH level is an early indicator of intravascular hemolysis [8,9,10]. Thrombocytopenia, intravascular hemolysis, elevated reticulocyte count, hyperbilirubinemia and low haptoglobin are characteristic findings. Complications include ARDS, congestive heart failure, DIC, renal failure, splenic infarct/rupture and warm autoimmune hemolytic anemia [6,7,11]. Our patient had severe Babesiosis requiring hemodialysis for AKI and seizure management. Kidney dysfunction is due to acute tubular necrosis from underlying sepsis, and heme pigment induced tubular injury [5]. Cerebral babesiosis (CB) occurs due to parasitized erythrocytes in the microvasculature and release of inflammatory mediators (2,3,4). Neurological manifestations include ataxia, paresis, muscle tremor, anisocoria, and vestibular signs (2,3). Diagnosis involves microscopic examination of Giemsa stained thin blood smears demonstrating intra erythrocyte trophozoites and serologic evidence. Treatment includes Atovaquone plus Azithromycin or Clindamycin with Quinine. In severe disease, RBC exchange transfusion is recommended [11,12].Prevention of babesiosis consists of personal protective measures to minimize tick exposure.
Conclusions: Despite being asymptomatic in majority of patients, Babesiosis can be life threatening resulting in shock, multiorgan failure, and sometimes even fatal. Prompt recognition in endemic areas and classic clinical presentation with laboratory findings and identification of intraerythrocytic parasite on blood smears can be lifesaving with appropriate antibiotic treatment.