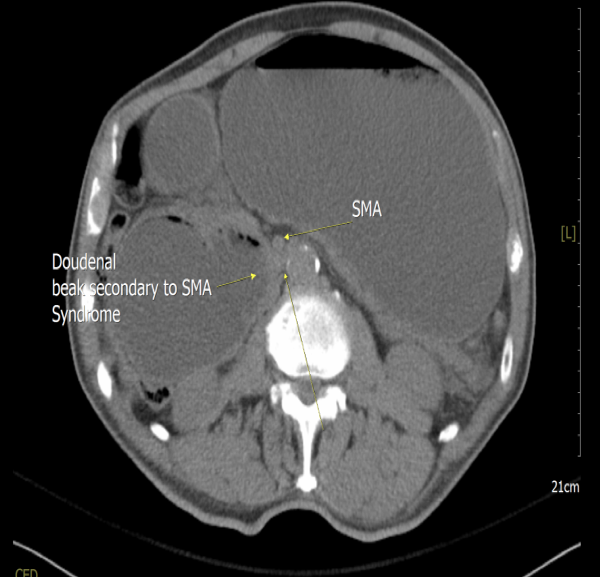
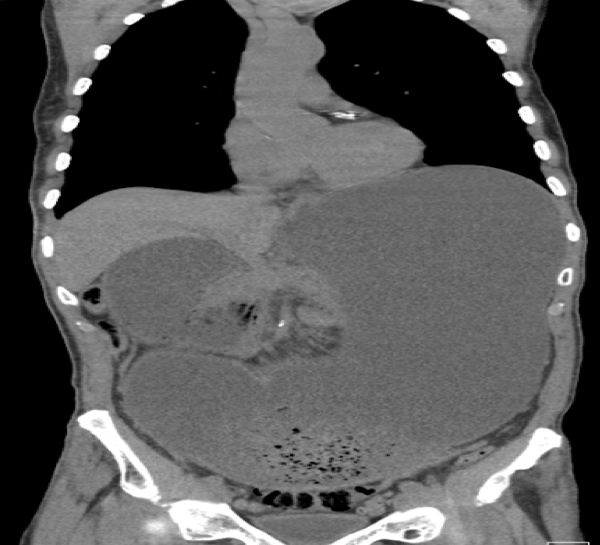
Case Presentation: An 83-year-old male with a history of hypertension and coronary artery disease presented to the ED with complaints of persistent hiccups for 1-week duration associated with drooling, decreased appetite, inability to lie flat, and significant weight loss over several months. He was hemodynamically stable and afebrile but noted to have diffuse abdominal tenderness with distension, firmness on palpation and hypoactive bowel sounds. Significant lab values were Cr 3.5 mg/dL, BUN 63 mg/dL, lactate 9.2 U/L, 11,500 white blood cells/UL and abdominal X-ray revealed mildly dilated air-filled loop of bowel in the right side of the abdomen. He was started on IV fluids and nasogastric tube was placed for suction and decompression. Given lactic acidosis in the setting of bowel obstruction and acute kidney injury, a CT abdomen and pelvis without IV contrast was done which revealed significant gastroduodenal distention to the level of the SMA at the 3rd portion of the duodenum (Figures 1 and 2). An upper endoscopy was done to rule out endoluminal causes of duodenal obstruction. However, endoscopy showed gastroesophageal reflux disease with esophagitis and extrinsic compression of the 3rd part of the duodenum, thus confirming a diagnosis of SMA syndrome.
Discussion: Superior mesenteric artery (SMA) syndrome is defined as an upper gastrointestinal mechanical obstruction caused by compression of the 3rd part of the duodenum between the SMA anteriorly and the aorta posteriorly that has an incidence of 0.1-0.3%. This is due to loss of the intervening mesenteric fat pad and classically seen in young females in anorexic or hyper-emetic states with rapid weight loss and progressively worsening postprandial epigastric pain, hiccups, abdominal fullness and vomiting. While SMA syndrome is typically treated with adequate nutrition, nasogastric decompression, and proper positioning of the patient after eating, this was not an option for this patient. Given the severe gastroduodenal distension, progressive weight loss, poor gastric motility and extensive fluid collection in the stomach, the patient underwent a gastrojejunostomy for gastric fluid drainage. There were no complications and he has remained asymptomatic for the past year.
Conclusions: This unique case stresses the importance of keeping a high clinical suspicion of SMA syndrome in the setting of severe weight loss with gastroduodenal distension and hiccups, as well as the prompt use of CT and endoscopy to diagnosis and assess the surgical approach.