Case Presentation:
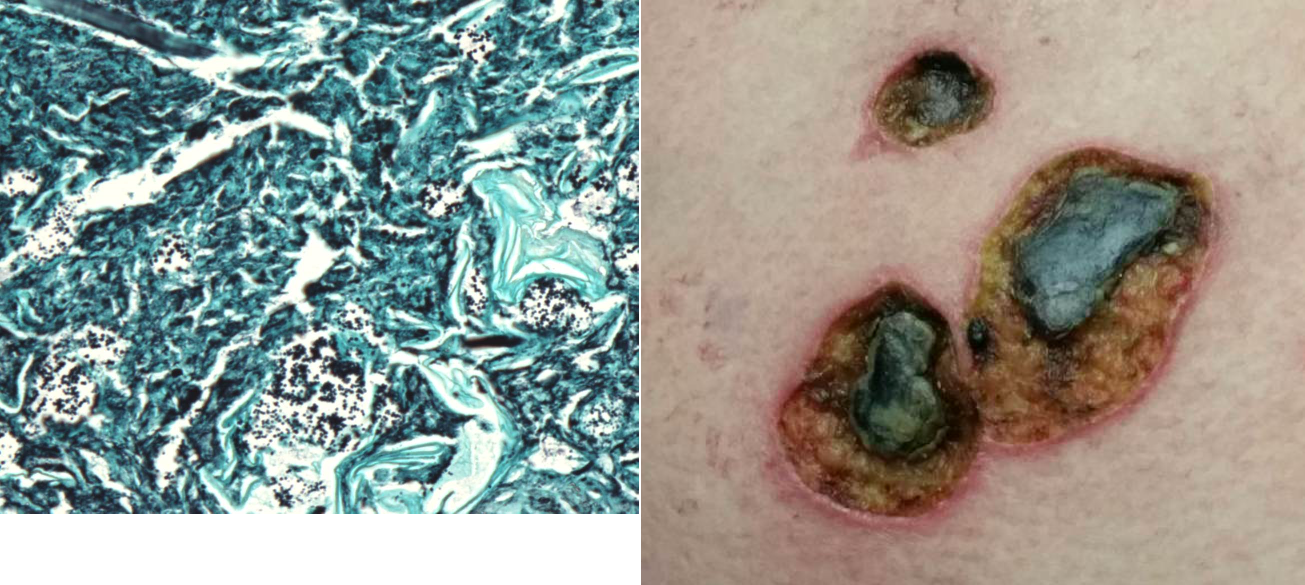
A 51-year-old woman with multiple medical co-morbidities including morbid obesity with body mass index of 84, hepatitis C cirrhosis, urinary retention requiring chronic indwelling foley catheter and bilateral non-obstructing renal calculi presented from her nursing home with altered mental status, tachycardia, hypotension, and urinalysis findings consistent with urinary tract infection. She had a prolonged history of recurrent multi drug resistant urinary tract infections with previous Proteus mirabilisbacteremia, likely secondary to her infected renal calculi; however, she was not an operative candidate due to her multiple co-morbidities. Several weeks prior to admission, she was treated empirically with ciprofloxacin and intramuscular gentamycin for presumed urinary tract infection by nursing home staff; however, her clinical status continued to worsen and she developed necrotic ulcers on bilateral upper extremities near her gentamycin injection sites (Figure 1).
On admission, she was started on meropenem and linezolid and initial urine and blood cultures grew out Proteus mirabilis. Dermatology was consulted for further evaluation of her necrotic skin ulcers and a punch biopsy illustrated acute inflammation and necrosis with florid bacterial organisms (Figure 2). Body tissue cultures from the ulcer sites grew Proteus mirabilis and Enterococcus faecalisand pathology was consistent with a diagnosis of ecthyma gangrenosum. A trans esophageal echocardiogram did not illustrate focal vegetation and she was treated with two weeks of intravenous meropenem. Urology was consulted for possible percutaneous nephrolithotomy, however the patient was again deemed a poor operative candidate and was ultimately transitioned to palliative care.
Discussion:
Ecthyma gangrenosum is a dermatologic finding of classically associated with Pseudomonas aeruginosa bacteremia in immunocompromised patients. Patients develop this rare finding when organisms colonize the media and adventitia of arteries or veins leading to local necrosis and ulceration of the epidermis and dermis. Although ecthyma gangrenosum has been associated with other bacteria and fungi, the majority of these case reports involve co-infection with Pseudomonas. Additionally, almost all documented case reports involve severely immunocompromised patients with HIV / AIDS, undergoing chemotherapy, or in the setting of acute leukemia.
Conclusions:
Ecthyma gangrenosum is an exceedingly rare dermatologic complication of bacteremia or fungemia. This case is particularly unique in that there was no co-infection with Pseudomonas species and our patient was not immunosuppressed. Additionally, our patient’s ulcers were initially misdiagnosed as an allergic reaction to intramuscular gentamicin injections, and an important sign of occult bacteremia was missed for several weeks. This report highlights an unusual case presentation and encourages physicians to maintain a broad differential diagnosis in the setting of unusual or atypical clinical presentations.