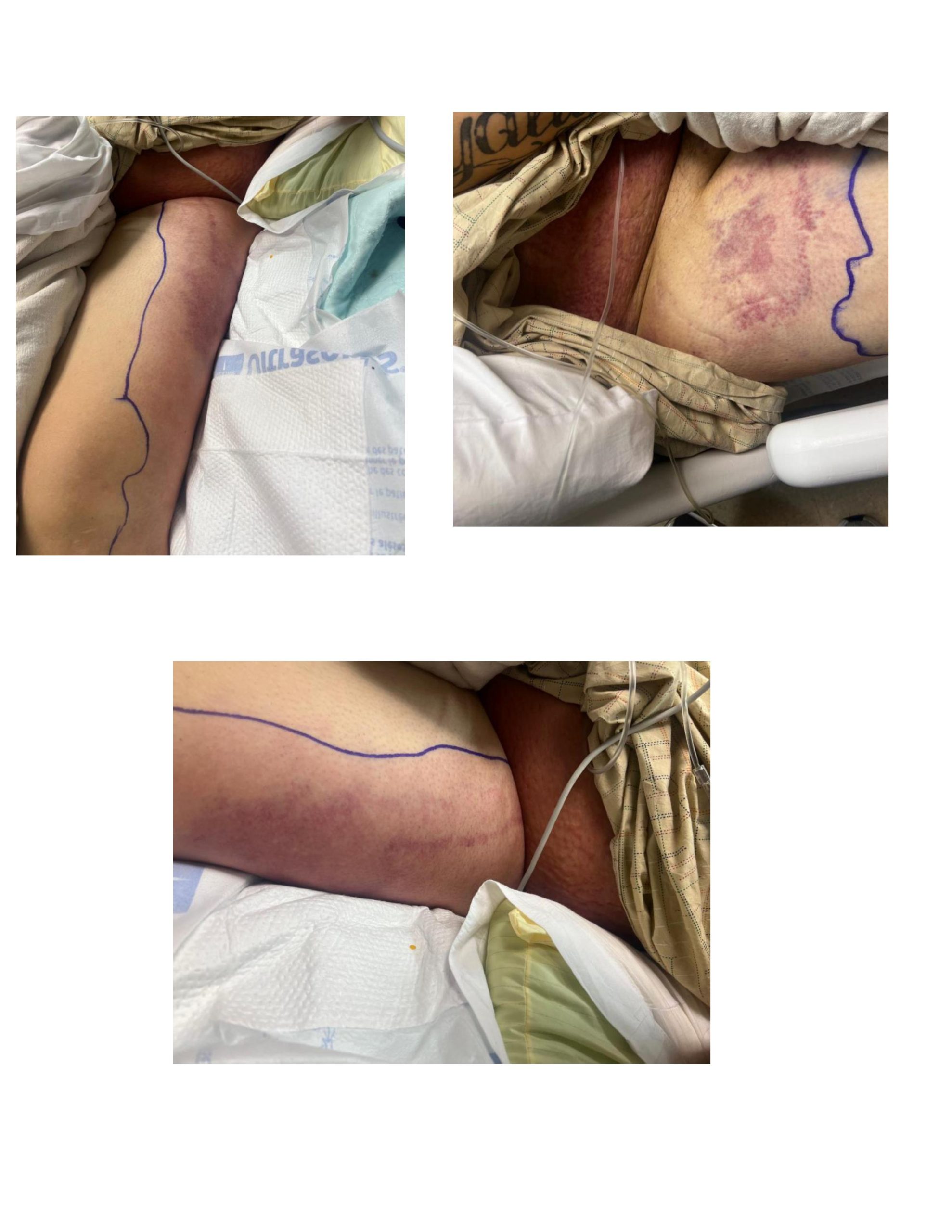
Case Presentation: A 24-year-old Hispanic male with morbid obesity, hypertension, hyperlipidemia, and class IV/V lupus nephritis on immunosuppressive therapy presented with a one-week history of progressive pain, erythema, and swelling in the lower abdomen and extremities. Symptoms included fever, shortness of breath, and diarrhea. Physical examination revealed a tender, erythematous rash with violaceous discoloration over the left lateral leg, groin, and proximal thigh, along with bilateral lower extremity edema. Vital signs showed tachypnea and tachycardia, necessitating high-flow oxygen support.Suspecting an infection, clinicians initiated broad-spectrum antibiotics after obtaining blood and stool cultures. Mycophenolate was temporarily discontinued due to concerns about its role in precipitating diarrhea.Laboratory findings revealed leukocytosis, lactic acidosis (2.5 mmol/L), elevated creatinine (6.0 mg/dL), and hyperkalemia (5.6 mmol/L). Imaging showed generalized edema, a small pleural effusion, and soft tissue changes consistent with cellulitis and myositis. Notably, no abscess was detected. Blood and stool cultures confirmed Salmonella as the causative pathogen, diagnosing Salmonella bacteremia and cellulitis. The patient responded well to IV antibiotics, including meropenem and clindamycin, with significant clinical improvement.
Discussion: Localized infections are recognized complications of Salmonella septicemia, particularly in immunocompromised individuals. However, skin involvement presenting as cutaneous lesions or cellulitis is rare. This case emphasizes the importance of maintaining a high index of suspicion for atypical pathogens like Salmonella in immunocompromised patients presenting with unusual skin findings. Early identification and treatment are crucial to prevent progression to severe complications, such as sepsis.
Conclusions: This case underscores the need for clinicians to consider Salmonella bacteremia as a potential cause of cellulitis or skin lesions in immunocompromised patients, particularly when common pathogens such as Staphylococcus or Streptococcus are excluded. Timely recognition, appropriate antimicrobial therapy, and careful adjustment of immunosuppressive medications are essential to improving outcomes and reducing morbidity in this vulnerable population.