Case Presentation: A 22-year-old woman with no known medical history presented with visual hallucinations, confusion, and jaundice. Her friend reported chronic nitrous oxide (N₂O) inhalation, escalating to three cans per day over the prior month. This increase coincided with a recent job loss and worsening mood. Days before admission, over 100 empty N₂O cans were found in her apartment. The patient was described as severely altered, mistaking her mother for a stranger and reporting seeing birds flying indoors.On admission, she appeared jaundiced but was alert and oriented to person, place, and time. She demonstrated difficulty with attention, concentration, and cognitive tasks. Neurological examination revealed ataxia, mild dysmetria, and decreased vibratory sensation in the toes. Initial laboratory studies revealed pancytopenia (WBC 1.2 × 10⁹/L, hemoglobin 7.4 g/dL, platelets 160 × 10⁹/L), elevated total bilirubin (4.9 mg/dL, indirect 4.3 mg/dL, direct 0.6 mg/dL), low haptoglobin (< 8 mg/dL), and elevated lactate dehydrogenase of 868 U/L. Vitamin B12 was severely deficient at < 148 pg/mL. A peripheral smear revealed macrocytosis with anisopoikilocytosis and features of ineffective erythropoiesis.Parietal cell antibodies were positive, supporting a diagnosis of pernicious anemia, while intrinsic factor antibodies were negative. The patient was treated with high-dose intramuscular vitamin B12. She demonstrated rapid improvement in her mental status. She was discharged with plans for continued B12 supplementation and close outpatient follow-up.
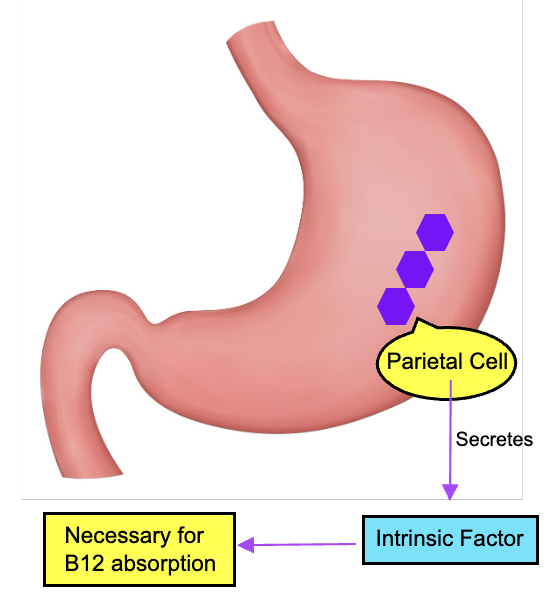
Discussion: This case highlights the layered causes of vitamin B12 deficiency, where N₂O use contributed to functional deficiency but was not the sole underlying factor. N₂O inactivates vitamin B12 by oxidizing cobalamin, leading to functional impairment. While neuropsychiatric effects of N₂O are well-documented, the combination of pancytopenia and hemolysis observed here is less typical and required further investigation.The detection of parietal cell antibodies confirmed pernicious anemia as an additional etiology. This autoimmune condition impairs intrinsic factor production and disrupts B12 absorption. The neuropsychiatric symptoms, including hallucinations, disorientation, and ataxia, underscore the systemic impact of severe B12 deficiency. Timely diagnosis and treatment, including high-dose B12 replacement, are essential to reversing these abnormalities and preventing irreversible complications.
Conclusions: Avoiding diagnostic anchoring and thoroughly verifying clinical features are essential for uncovering complex cases. While functional B12 deficiency from N₂O use was a clear contributing factor, further investigation revealed pernicious anemia as a coexisting autoimmune process. This discovery was critical to understanding the full scope of the patient’s hematologic and neuropsychiatric findings and ensuring appropriate treatment.Staying open to alternative explanations allowed the team to connect the dots. It’s easy to stop after finding one answer, but this case demonstrates the value of digging deeper to uncover critical findings. A broad, thoughtful approach not only leads to better outcomes but also cultivates the clinical insight that defines great medicine.