Case Presentation:
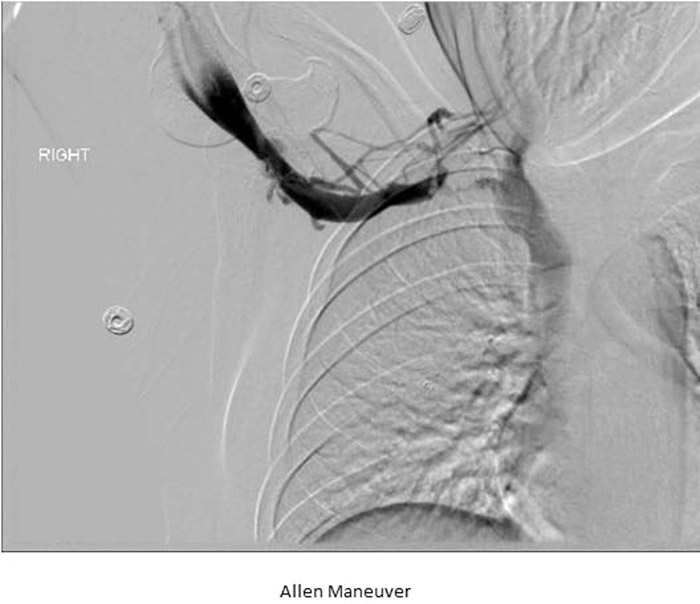
A 20 year old female, presented with swelling, numbness and pain of her right arm for the past 2 days. She gave a history of competitive swimming in college. One morning she noticed her right arm was swollen, blue, painful and slightly numb. On exam there was swelling over the right upper limb, neck, axilla and infra‐clavicular area, with mild discoloration and moderate tenderness. Ultrasonography showed findings consistent with a thrombus within the subclavian and axillary veins. CTA revealed there being small pulmonary embolisms of the right lower lobe. Hypercoagulable workup were negative for any secondary causes. She went for a right upper extremity/superior vena cava venogram catheter directed pharmacologic thrombolysis. After 24 hours of local TPA infusion, a repeat IR guided right upper chest venogram demonstrated near resolution of the thrombus. Provocative maneuver, known as the Allen Maneuver, where the patient’s arm is extended over the head in the abducted position was performed, which demonstrated abrupt cutoff within the right subclavian vein. Findings compatible with Paget‐Schrodder Syndrome (PSS) (Image 1). She was discharged on full dose Lovenox for six months with planned outpatient procedure for removal of the first rib.
Discussion:
Upper‐extremity deep vein thrombosis (UEDVT) is thrombosis of the axillary and/or subclavian veins. Primary UEDVT is rare, and refers to effort thrombosis or PSS. Secondary UEDVT, which is more common, is seen in older population with co‐morbidities, malignancies or central venous catheters. UEDVT complications include pulmonary embolism, persistent pain/swelling, superior vena cava syndrome and vascular access issues. Young, healthy patients with PSS develop spontaneous UEDVT, after strenuous activities such as playing sports. Exertion causes microtrauma to the vascular intima leading to activation of the coagulation cascade. Also, the axillary subclavian vein traverses the tunnel formed by the clavicle, subclavicus and scalenus anticus muscle, first rib and costoclavicular ligament. Abnormalities to these structures; may narrow the tunnel leading to thrombosis. Complaints include heaviness, mild dull ache/pain in the neck, shoulder and/or axilla, ecchymosis/swelling, discoloration/mottled skin and distention of the cutaneous veins. Traditionally treatment was limb elevation and anticoagulation. Now, catheter directed thrombolytic therapy followed by transaxillary first rib resection, have been the treatment of choice. The majority of patients improve overtime; however, some patients suffer from a post‐thrombotic syndrome due to chronic venous insufficiency.
Conclusions:
Our patient developed a thrombus in her dominant arm without any effort, which is an unusual presentation for PSS. Secondary causes were ruled out and after a venogram, the proper diagnosis of PSS was made. She was a young, competitive swimmer and likely had repeated strenuous activity involving hyperabduction at the shoulder, damaging the vessels and causing hypertrophied muscles which compress on the vessel. It is interesting to note in this case that her thrombus formed effortlessly, which is very uncommon in patients with PSS. She had not swam in many months and developed a thrombus only after waking up. It appears, based on this case, that PSS should be considered in all patients, depsite the history of effort use or not