Background:
In recent years, our institution has faced challenges in meeting our health system’s rigorous targets for CMS Core Measures for Heart Failure (HF). Our overall Appropriate Care Score for HF, while exceeding the national average, has lagged behind the other hospitals in our health system. Our scores have largely been driven by the HF‐1 measure, which deals with HF‐specific discharge instructions. Barriers to achieving our HF targets have included transcription errors, inconsistencies in medication reconciliation, and incomplete or missing discharge documentation. Improving our performance in discharge documentation for HF patients will help us provide the highest quality patient care, and will result in better adherence to publicly reported quality metrics, including the CMS Value Based Purchasing Clinical Process of Care domain.
Purpose:
Our goal was to develop and implement strategies to improve the accuracy and completeness of discharge documentation for HF patients, and thereby improve our quality of care as well as our HF‐1 adherence and our overall Appropriate Care Score for Heart Failure.
Description:
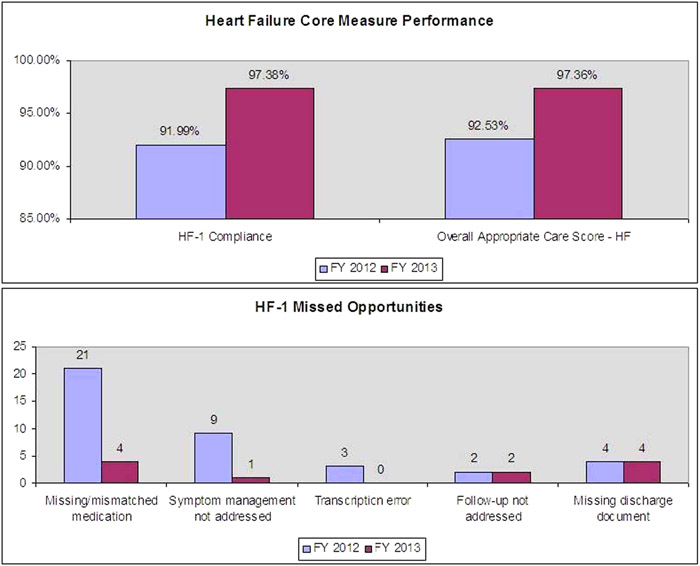
We implemented three strategies to improve the quality and accuracy of our discharge documents for HF patients. First, we added functionality within our electronic medical record to facilitate insertion of specific heart failure instructions into all discharge instruction templates. This strategy was intended to reduce the number of patients who did not receive written instructions addressing diet, activity, weight monitoring, and HF symptom management. Second, we drafted and gained approval of a hospital policy requiring providers to dictate discharge medication lists in discharge summaries using the same medication list given to patients at the time of discharge. This strategy was intended to improve the accuracy of the discharge medication reconciliation process and to ensure that all patients (not just HF patients) and their primary care providers received an accurate list of medications at the time of discharge. Third, we implemented a documentation review process for HF discharges, including physician to physician communication addressing any correctable deficiencies such as transcription errors, dictation errors, or ambiguous documentation. After implementation of these three strategies, our compliance with HF‐1 increased from 91.99% in FY 2012 to 97.38% in FY 2013, and our overall Appropriate Care Score for HF increased from 92.53% in FY 2012 to 97.36% in FY 2013.
Conclusions:
Implementing the three strategies discussed above resulted in an increase in the completeness and accuracy of discharge instruction documents for HF patients, and improvements in both compliance with the HF‐1 measure and the overall Appropriate Care Score for Heart Failure. Given the complexity of HF discharge documentation, a multi‐faceted approach is likely to be necessary at other institutions seeking to improve their performance in this area