Background:
Research shows that continuity of care in the outpatient setting improves care and reduces risk of rehospitalization. However, the effects of continuity of care in the inpatient setting have not been studied. We know that the growth of hospitalists with rotating schedules and night float services often lead to 1 physician admitting the patient and another caring for the patient during a hospitalization. We sought to determine whether continuity of care by 1 physician during hospitalization affects patient outcomes including adverse events, length of stay (LOS), and risk of rehospitalization or emergency department visit postdischarge.
Methods:
We conducted a retrospective chart review of all general medicine patients admitted to the hospitalist service between January 1, 2008, and October 31, 2008. For our interim analysis, we chose 109 sequential admissions in January, 147 in April, and 167 in August to reflect 3 points in the academic year. The final analysis aimed to review approximately 4000 charts. Patients were excluded if they were directly admitted to the intensive care service, surgery services, or hematology/ oncology services to prevent including patients with critical illness, surgical complications, or chemotherapeutic needs, respectively. Of the 423 charts reviewed, 402 met inclusion criteria. Charts were reviewed to determine whether continuity of care was present over the course of admission. Continuity was present if the admission history and physical was written by the same physician who wrote a progress note on the patient the following day. Additional outcomes of interest included length of stay, poor outcome within the first 24 hours of admission (defined as ICU transfer, cardiac arrest, or death), hospital charges, and repeat visits to the emergency department or readmissiors within 30 days of discharge. Differences in results were assessed with a chi‐square analysis for categorical variables and the t test for continuous variables.
Results:
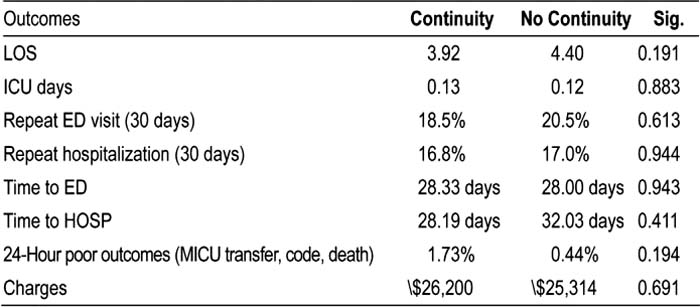
Among the 402 inpatient admissions evaluated, 173 patients (43.0%) were admitted and followed up by the same physician. Overall, 55.6% were female, and the average age was 60.8 years, with no significant difference between the groups. There were no significant differences between the continuity versus no‐continuity patients for LOS — 3.92 versus 4.40 days (P = 0.2), poor outcomes 1.73% versus 0.44% (P = 0.2), repeat visit to the ED within 30 days of discharge (P = 0.6), rehospitalization within 30 days of discharge (P = 0.9), and hospital charges $26,200 versus $25,314 (P= 0.7). This remained true after adjusting for case‐mix index.
Conclusions:
Continuity of care, as defined by having the same physician who admitted the patient perform initial follow‐up in the inpatient setting, does not appear to result in more favorable patient outcomes in length of stay, risk of poor outcomes, or risk of rehospitalization.
Author Disclosure:
R. Khanna, none; A. Marouni, none; L. Lindquist, none; J. Feinglass, none; D. Wayne, none; M. Williams, Society of Hospital Medicine, Journal of Hospital Medicine Editor; K. Wachsberg, none.