Background: After a patient death, experienced physicians have reported feelings of sadness, guilt, and self-doubt. Residents and interns experience a strong emotional impact to these deaths as well, and previous studies have shown that they only feel adequately supported 50% of the time. Residents feel more supported by their attendings and are better able to emotionally cope if debriefs occur after adverse events or deaths. There are few studies on how frequently hospitalists hold debriefs after patient deaths and how best to conduct such discussions.
Purpose: The purpose of the study is to understand current practices in coping with patient deaths and to create a debrief tool to guide residents and hospitalists in conducting debriefs after a patient mortality or adverse event.
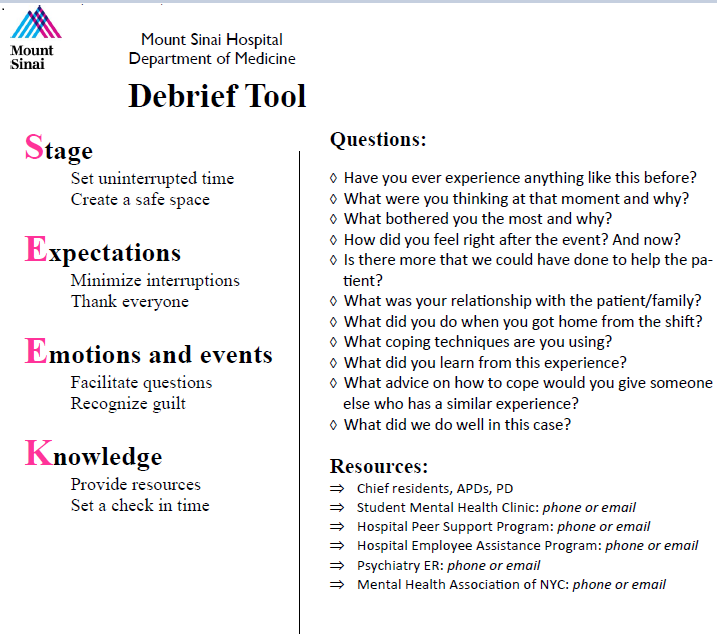
Description: The study was conducted at a large urban academic medical center. An initial anonymous survey was administered to Internal Medicine residents and hospitalists to understand current debrief practices. There were 13 hospitalist respondents and 31 resident respondents. The survey found that debriefs do not happen consistently, with only 31% of hospitalists reporting that they always debrief after a patient death or adverse event and 0% of residents reporting that their attending always leads debriefs. Although 77% of hospitalist respondents reported recognizing when trainees are having difficulty coping with a patient death or adverse event, only 55% of residents agreed that their attendings recognized that they were having difficulty coping. Furthermore, 65% of resident respondents reported that they were not aware of mental and emotional health resources and 69% of hospitalists reported that they have never provided such resources. Survey data also showed that 100% of the hospitalists had not received training on how to conduct debriefs, but 100% would want a tool to help them debrief.A debrief tool was created based on the need indicated from the survey (figure 1). Specific elements were selected from best practices when discussing difficult events and from a survey question related to physician perception of the purpose of debriefs. Further input was taken from focus groups of residents and hospitalists. Using the mnemonic SEEK, the tool emphasizes the following 4 components: Setting a stage, creating Expectations and a blame-free environment, discussing Emotions and providing additional Knowledge and resources. This tool also includes sample questions to guide the discussion when leading a debrief and resources for emotional and mental care. Laminated cards with the tool were published and made available online. Training sessions were conducted with both residents and hospitalists, and they were guided through elements of a debrief, sample questions to facilitate discussion, and how to use the tool. At the end of the training session, hospitalists and residents applied their newly learned skills to challenging clinical scenarios.
Conclusions: The development and implementation of a tool helped to establish an easily adopted method to facilitate debriefs. Follow-up comments from attendings and residents have shown that debriefs are occurring more frequently after adverse events and deaths, and that they have been helpful and very much appreciated by the residents. Further evaluations and results will need to be collected. Additionally, applying the tool to specialty services, in ICUs, and continuing to train additional residents and hospitalists will broaden the practice of debriefs.