Case Presentation:
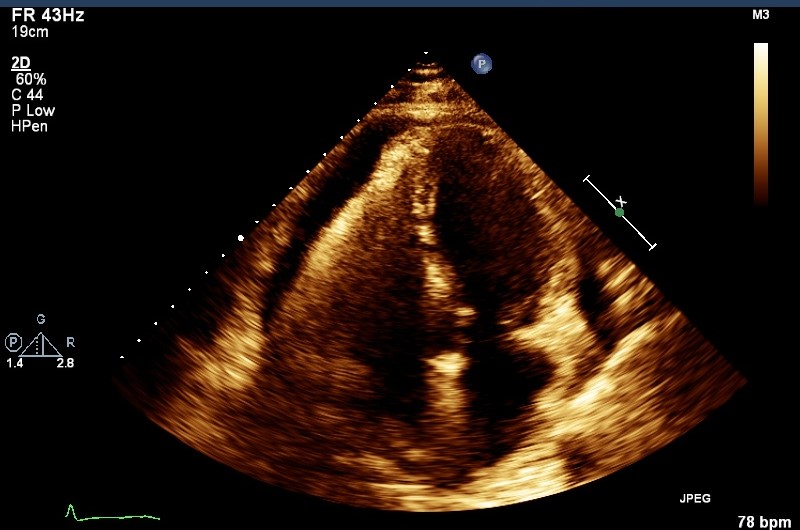
69-year-old gentleman presented to the emergency room with 6-week history of progressive dyspnea, lower limb edema and weight gain. Patient had a relevant past history of melanoma on the scalp treated with surgery, orthotic liver transplant, diabetes mellitus, chronic kidney disease stage two and hypertension. Patient denied viral prodrome, new drug initiation, sick contacts or trauma. Physical examination revealed jugular distension, pedal edema and rales but no murmurs/rubs, rashes, lymphadenopathy and benign neurological exam. Laboratory data revealed WBC 2.2, platelets 61, creatinine 1.5mg/dl, BUN 23mg/dl, TSH 1.8uIU/ml, BNP 83pg/ml. Chest radiography showed atelectasis/consolidation. Computerized tomography was performed which showed a large pericardial effusion and tamponade was ruled out with echocardiography. Further tests revealed ESR 73mm/hr., CRP 138mg/L, low C3, C4, ANA 1:640, positive anti-histone and negative respiratory virus panel, SSA, SSB, ANCA, ds-DNA, anti-Smith, HIV. Thoracic surgery performed aspiration of 500cc fluid with biopsy and window placement. Cytology showed acute inflammatory cells and biopsy was positive for acute and chronic pericarditis, no malignancy. Patients’ hydralazine dose had recently been increased to total 300mg/day which increased suspicion of drug induced lupus. Hydralazine was discontinued and a repeat echo performed after four weeks was negative for re-accumulation of effusion.
Discussion:
Few case reports describe effusions due to drug induced lupus per our literature review. Drugs like minocycline, hydralazine, and procainamide are implicated but the entire list is extensive. The patho-physiology is unclear, but non-specific activation of T cells, cytotoxic metabolites, drugs acting as haptens and acetylation status are implicated. Hydralazine can have a dose dependent effect for causing lupus and has also known to cause vasculitis with glomerulonephritis. There are no definitive diagnostic criteria or tests for drug induced lupus. Patient should have some symptoms of lupus with history of implicating drugs but not all criteria of SLE are required. Discontinuation of medication usually resolves the condition and re-challenge of drug should not be attempted. Resistant cases may require anti-malarial or glucocorticoids.
Conclusions:
Hydralazine is a commonly used medication to treat moderate to severe hypertension. About 5-10% of drug-induced lupus is caused by Hydralazine. Thus, hospitalists should be cognizant of this complication, especially with atypical presentations in an immunosuppressed state as demonstrated in this case. Furthermore, if the patient has a history of drug-induced lupus, re-challenging the offending agent should not be attempted.