Background: Racial/ethnocultural inequities have been demonstrated throughout our health care system, though their presence among patients who undergo interhospital transfer (IHT), commonly done to provide patients with more specialized care, is poorly understood. The goals of this study are to evaluate the association between patient race/ethnicity and IHT to identify potential racial disparities in this care transition.
Methods: We performed a retrospective analysis using 2016 data from the National Inpatient Sample (NIS), the largest publicly available all-payer inpatient health care database in the United States which yields national estimates of hospital inpatient admissions. All adult patients ≥ age 18 were included. The primary outcome was IHT, defined as transfer to another acute care facility. The primary predictor was race, categorized as traditionally underserved racial/ethnic minority groups (Black, Hispanic, Native American) versus other (White, Asian, Other). We performed univariate, then multivariate logistic regression models to obtain the adjusted odds of IHT by race, adjusting for patient and hospital characteristics, including patients’ age, sex, insurance, median household income by zip code, mortality risk by diagnosis-related group (DRG), hospital teaching status, region and number of annual discharges. We performed secondary analyses using individual race/ethnicity categories.
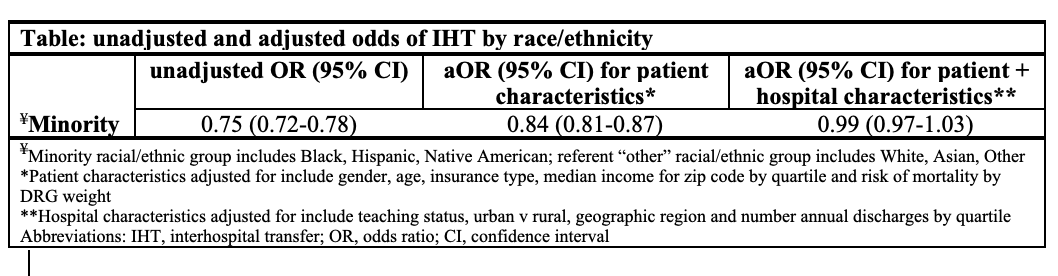
Results: There were a total of 6,037,727 unique admissions in the cohort, among whom 120,396 (2.39%) were transferred to an acute care facility. Among those transferred, 46.2% were female, 72.7% were white, 13.3% were Black and 8.4% were Hispanic. Univariable analysis revealed that minority patients had a lower odds of transfer compared to other groups (OR 0.75, 95% CI 0.72-0.78). Multivariable logistic regression adjusting for patient characteristics also revealed a lower odds of transfer (OR 0.84, 95% CI 0.81-0.87). However, when we additionally adjusted for hospital characteristics, this association lost significance (Table). In secondary analysis, Hispanic ethnicity was associated with lower adjusted odds of transfer compared to White patients (OR 0.94, 95% CI 0.90-0.98).
Conclusions: In this nationally representative sample of patients undergoing IHT, we found that minority race/ethnicity, and Hispanic ethnicity in particular, was associated with lower odds of IHT. These findings remained after adjusting for patient characteristics, but became non-significant after also adjusting for hospital characteristics, suggesting that existing racial disparities may be mitigated in part by factors affecting the hospitals to which minority patients present. Additional research is needed to further explore the drivers of these inequities.