Case Presentation: A 54-year-old man presented with confusion, vomiting, and weakness. En route to hospital he received dextrose for a glucose of 40. Admitted to the ICU for severe metabolic acidosis. Past medical history included type 2 diabetes, depression and PTSD. Aside from tachycardia, smell of alcohol, and bilateral hand tremor, initial physical exam was documented as normal. Notable admission labs included bicarbonate 9 (anion gap 22), lactic acid 16 (reference range 0.5-2.2), mild beta-hydroxybutyrate elevation 0.69 (reference range <0.27) and VBG pH 6.887, pCO2 32. Blood ethanol level was 193. Negative toxic alcohols, salicylate and acetaminophen levels.
He was treated with dextrose, saline, bicarbonate drip, CIWA and IV thiamine for alcohol withdrawal. Lactic acidosis resolved within 10 hours. He was transferred to floor with a working diagnosis of “lactic acidosis, likely due to metformin toxicity.”
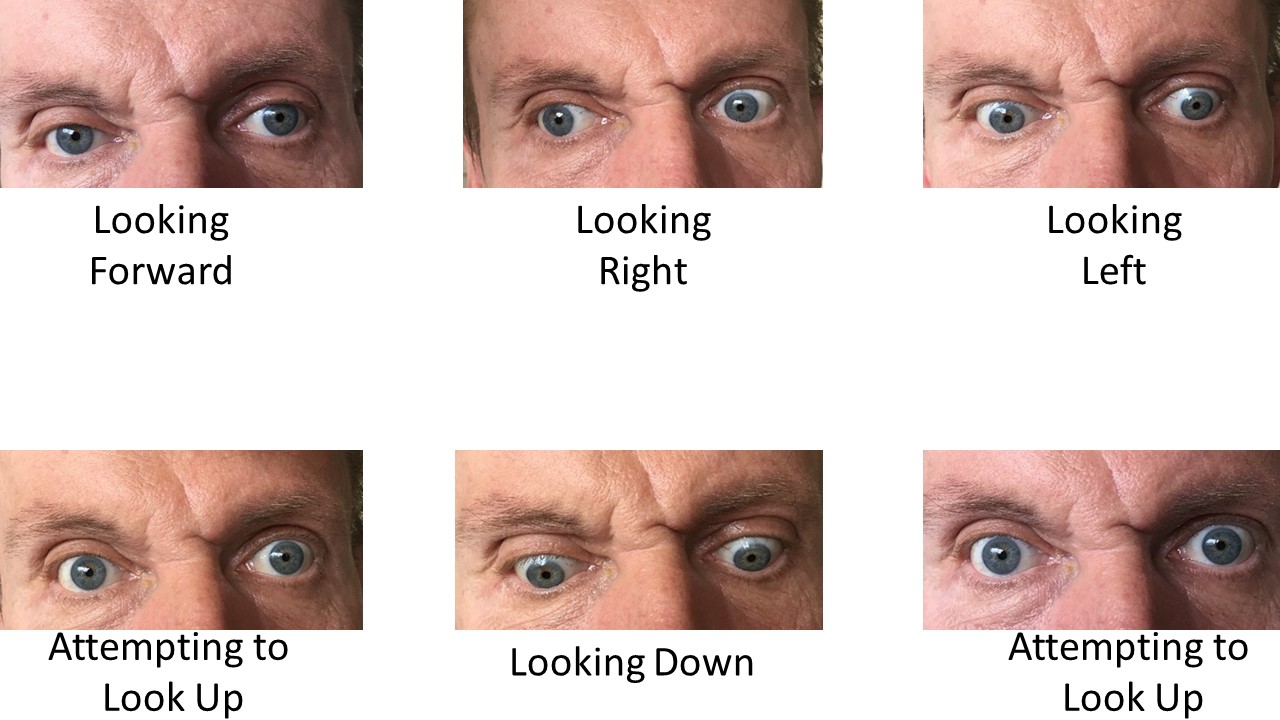
Upon transfer his exam was notable for extensive scarring of the abdomen, which he said was due to shrapnel and intestinal resection during the Soviet war in Afghanistan. Neurologic exam with profound symmetric lower extremity weakness, decreased patellar reflexes but hyper-reflexive upper extremities, severe ataxic uncoordinated gait, and inability to perform upward gaze.
He reported being a former Russian military officer, a “political refugee” from the Soviet Union, and stated: “I think I have been poisoned!”. In context of recent assassination attempt of a KGB officer in London with a nerve agent, the working diagnosis was re-visited.
Discussion: The combination of malabsorption, from intestinal resection and alcohol abuse, likely led to chronic thiamine deficiency. Dextrose prior to thiamine repletion triggered acute metabolic crisis. Thiamine is critical to aerobic metabolism in the Krebs cycle as a key co-factor to pyruvate dehydrogenase and alpha-ketoglutarate dehydrogenase. Acute fulminant thiamine deficiency, called “Shoshin beriberi,” can lead to severe systemic lactic acidosis. Thiamine replacement typically causes rapid resolution of lactic acidosis. Thiamine deficiency can also induce brain and nerve injury seen in this patient as Wernicke’s triad: altered mental status, ataxia, and ophthalmoplegia.
Conclusions: With ongoing thiamine repletion, the lactic acidosis resolved, his neurologic deficits improved, and he discharged with ongoing thiamine replacement. The combination of nutritional deficiency risk, neurological deficits, and lactic acidosis should raise suspicion for Shoshin beriberi. No KGB assassins were required to explain the clinical presentation.
Key Points:
-Thiamine deficiency is an easily overlooked etiology of severe lactic acidosis.
-Thiamine prior to glucose is critical to avoid precipitating crisis in high risk patients.
-Transitions of care are a chance to re-evaluate operating hypotheses and recognize clinical syndrome evolution.