Case Presentation: A 24-year old woman presented to the emergency department with three days of decreased vision after she sustained blunt trauma to her face during a physical altercation. Social history was notable for methamphetamine use and unprotected sexual activity with multiple partners. Physical exam demonstrated right-sided periorbital swelling and tenderness, pupils were equal, round, and reactive to light, with no conjunctival injection, neck stiffness, rash, or difficulty ambulating. Labs were notable for white blood cell count 13.2 x 109/L, urine toxicology positive for amphetamines, and a negative HIV screen.
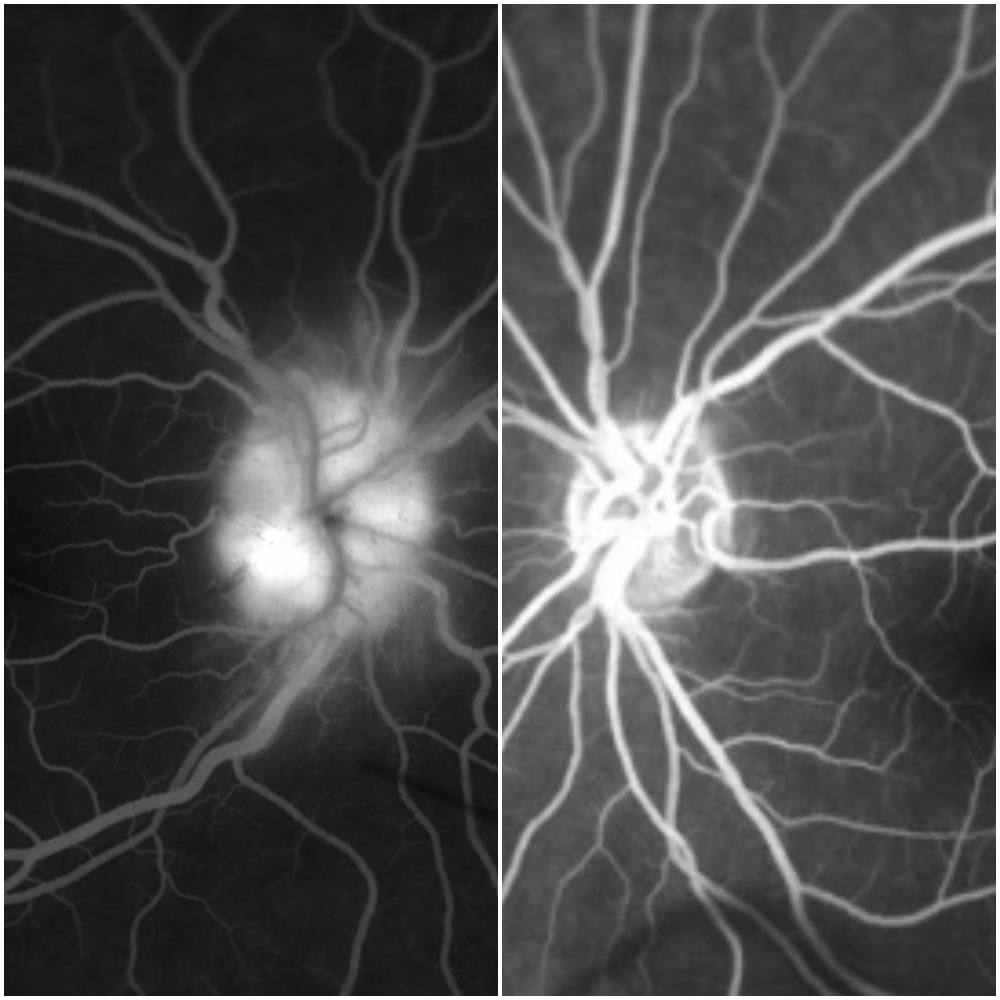
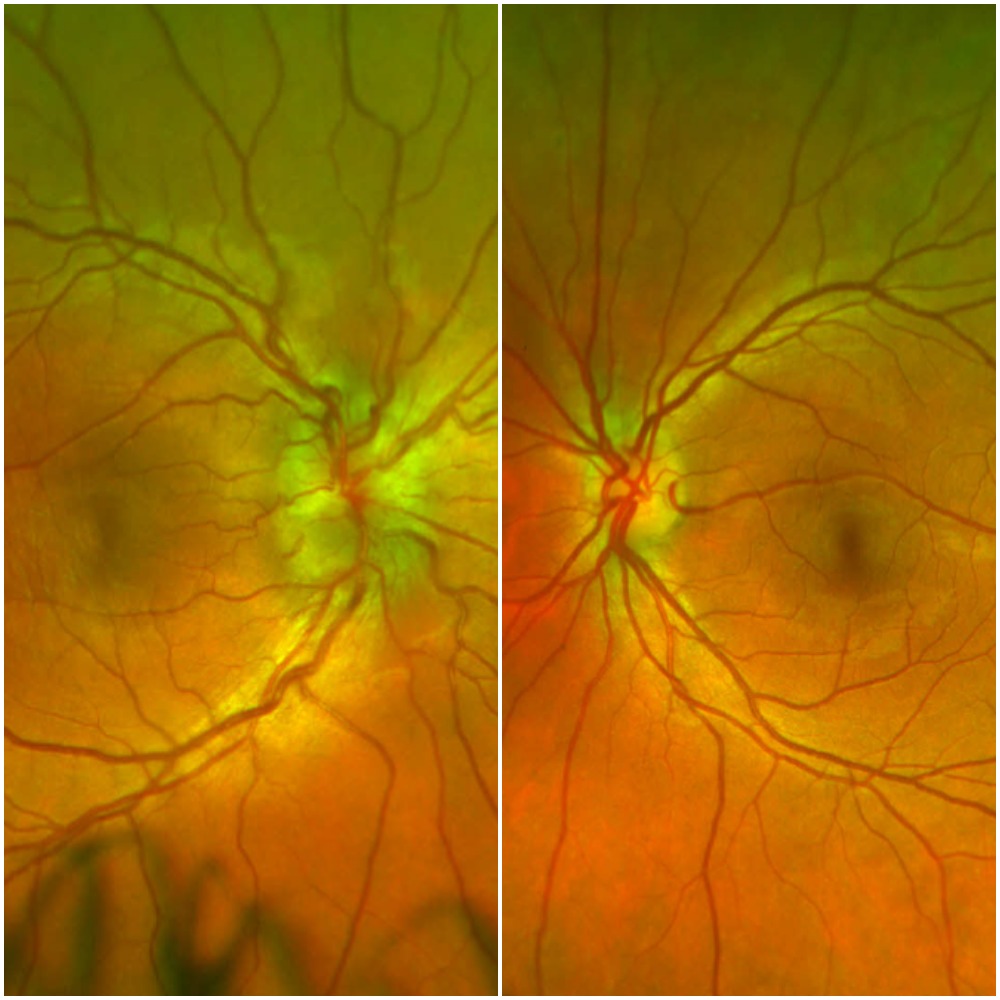
A maxillofacial CT showed right preseptal cellulitis with a small abscess. Wound cultures from an incision and drainage grew MRSA sensitive to TMP/SMX, which began resulting in improved periorbital swelling and decreased pain. Despite this improvement, the patient continued to complain of decreased visual acuity in her right eye that eventually progressed to both eyes on hospital day four. Ophthalmology was consulted and a dilated fundoscopic exam revealed bilateral, asymmetric optic disc swelling and optic papillitis. An orbital MRI revealed bilateral optic neuritis. A lumbar puncture was subsequently performed that revealed an opening pressure of 14 cmH2O, glucose 51 mg/dL, protein 43 mg/dL, nucleated cell count 2 cells/cumm, and a non-reactive VDRL. Serum studies demonstrated an RPR titer 1:128, reactive T. pallidum antibody, and reactive FTA-ABS, leading to the diagnosis of isolated ocular syphilis. The patient was started on aqueous penicillin G at 4 million units IV q4h for 10 days and penicillin G benzathine 2.4 million units IM weekly for 3 weeks. The patient completed three days of treatment with improved symptoms before leaving the hospital against medical advice.
Discussion: Isolated ocular syphilis is an uncommon presentation of neurosyphilis, especially among HIV-negative patients. Although classically associated with syphilitic meningitis, ocular syphilis can present independently during any stage of syphilis. It can also develop occultly, as was seen in our patient, whose diminished visual acuity was initially attributed to her recent trauma. Ocular syphilis most commonly presents as posterior uveitis and panuveitis. The most common presenting symptoms include diminished visual acuity, eye redness, and blurry vision. The treatment for neurosyphilis and ocular syphilis is 18-24 million units of Penicillin G daily for 10-14 days.
Conclusions: Given the increasing rate of syphilis in the US and morbidity associated with untreated syphilis, hospitalists should remain cognizant of the signs and symptoms of ocular syphilis in order to prevent delay in treatment. Regardless of the patient’s HIV status, ocular syphilis should be suspected in at risk patients who present with visual complaints.