Case Presentation: Statins are commonly prescribed medications that reduce cardiovascular disease. Their side effect profile consists of muscle-related adverse effects that are classified into toxic or autoimmune forms. We present a case of statin-induced necrotizing autoimmune myopathy (SINAM), a recently characterized entity within this spectrum of statin myotoxicity. While rare, it is important to recognize SINAM as a potential side effect of statin use and identify the main constellation of findings that characterize it.
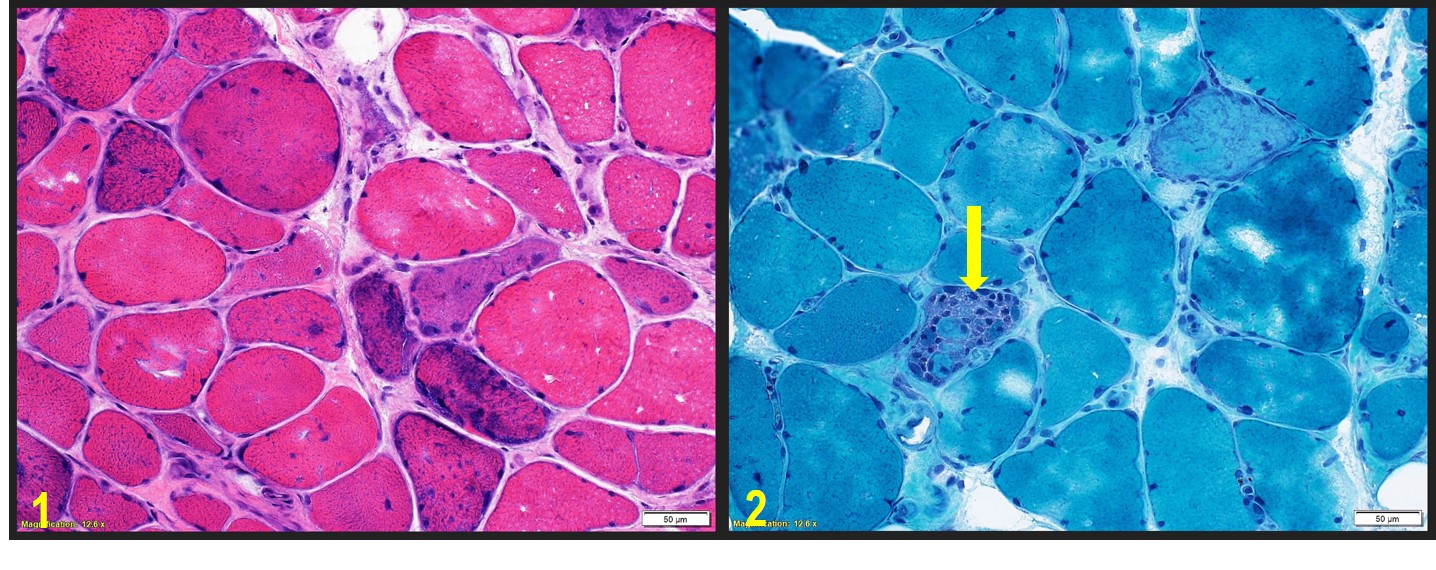
A 58-year-old African American man with a history of cervical spondylosis, diabetes, hyperlipidemia presented with lower extremity swelling and progressive leg weakness following a fall one month prior whereby his legs “gave out”. He had been restarted on atorvastatin 1 year prior, which had initially been discontinued for muscle spasms then deemed unrelated. Physical exam was significant for 3+ edema of lower extremities bilaterally to thighs and proximal muscle weakness with strengths of 4/5 in biceps/triceps but 3/5 in hip flexors/extensors. Pertinent workup for his weakness revealed a benign endocrine workup, normal inflammatory markers (ESR 12, CRP 0.26), negative myositis panel, but a positive ANA, greatly elevated muscle markers (Aldolase 66, CK 11,635), and a high titer positivity for Anti-HMG CoA Reductase (>200). MRI femur showed increased signal within proximal posterior and medial muscle groups indicative of compartmental myositis and skeletal muscle biopsies revealed a necrotizing myopathy with a paucity of chronic inflammation. The patient was started on prednisone 50mg daily, all statins added as allergies, and was discharged with close rheumatology follow up. Given his continued falls despite intense physical therapy, mycophenolate and IVIG were added, with improvement in strength and edema, a downtrend of his CK to 400, and the ability to taper him off prednisone.
Discussion: The pathogenesis of SINAM is via the marked up-regulation of the hydroxy-3-methyglutaryl-coenzyme A reductase receptor protein (HMGCR) in regenerating muscle cells of susceptible persons when exposed to statins, which then act as autoantigens to induce antibody production. The anti-HMGCR antibody then triggers necrosis and regeneration of muscle fibers, resulting in severe muscle damage that persists even after the discontinuation of the statin. SINAM is characterized by significant proximal muscle weakness, CK levels over 6000 U/L, evidence of muscle-cell necrosis on biopsy with minimal inflammatory infiltrates, and the presence of autoantibodies against HMG-CoA reductase as demonstrated in our patient case. Treatment includes discontinuing the statin, with half of all patients needing triple therapy consisting of high dose prednisone and two immunosuppressive agents. When recognized and treated, most patients have good outcomes.
Conclusions: While inflammatory myopathies are rare, with SINAM having an incidence of 2 out of 100,000 persons on statins, given the large prevalence of statin use, the importance of early recognition and appropriate management of this debilitating condition cannot be under emphasized.