Background: The discharge process is complex and high-risk. Clear and accurate communication between the physician or Advanced Practice Provider (providers), nurse, and patient are essential to ensure a safe and effective transition of care. Upon literature review, there have not been studies looking at interprofessional communication during the discharge process. Also, our institution (a large tertiary academic medical center) does not have a formal communication plan at the time of discharge. This study focused on understanding the current discharge practice to identify barriers in communication that may impact the quality of discharge care.
Methods: The study team analyzed communication on the general medical floors between provider, nurse, and patient at the time of discharge. This was done via a multifaceted approach. Nurses and providers on the primary general medicine floors were surveyed about their satisfaction with and barriers to communication in the current discharge process. The study team also observed the discharge process from a provider, nurse, and patient perspective, taking notes that were used for qualitative analysis. Providers and nursing staff were also interviewed about current discharge communication.
Results: There were 97 responses to the survey with participation from attending physicians, Advanced Practice Providers, senior residents, interns, and nurses (22.61%, 2.06%, 19.59%, 8.25%, 48.45% respectively). Providers ranked satisfaction with discharge communication as 3.35/5.00 while nurses ranked it 2.67/5.00 (p=0.0003). When nurses were asked how they currently are notified of the discharge plan, 76.92% responded by discharge orders in the EMR while 94.87% preferred direct communication or a phone call with the provider. Qualitative analysis of the interviews with providers and nurses showed several themes including nursing staff unable to round with providers, ineffective phone calls between nurses and providers, and nurses feeling uninformed of the discharge plan.
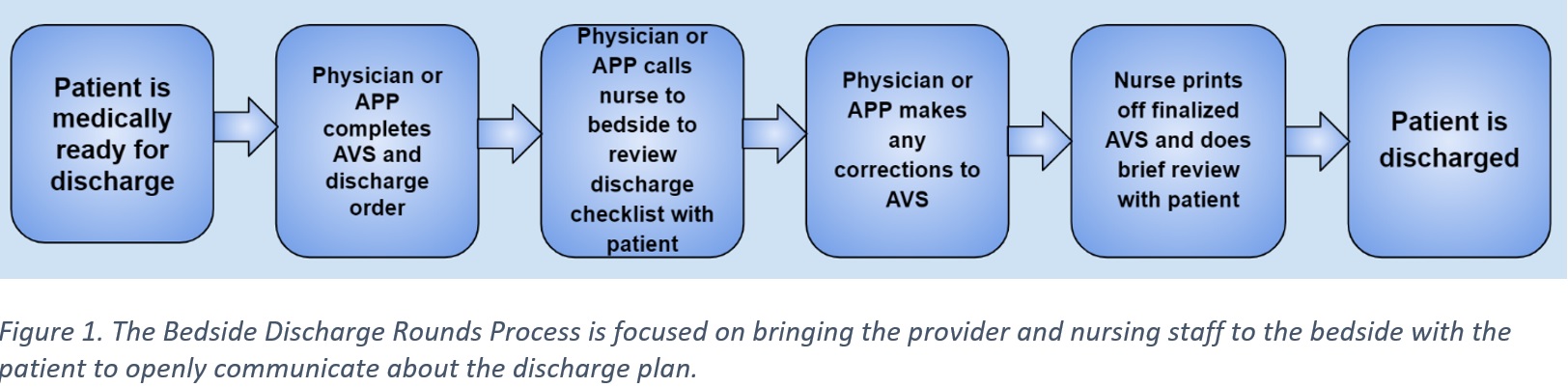
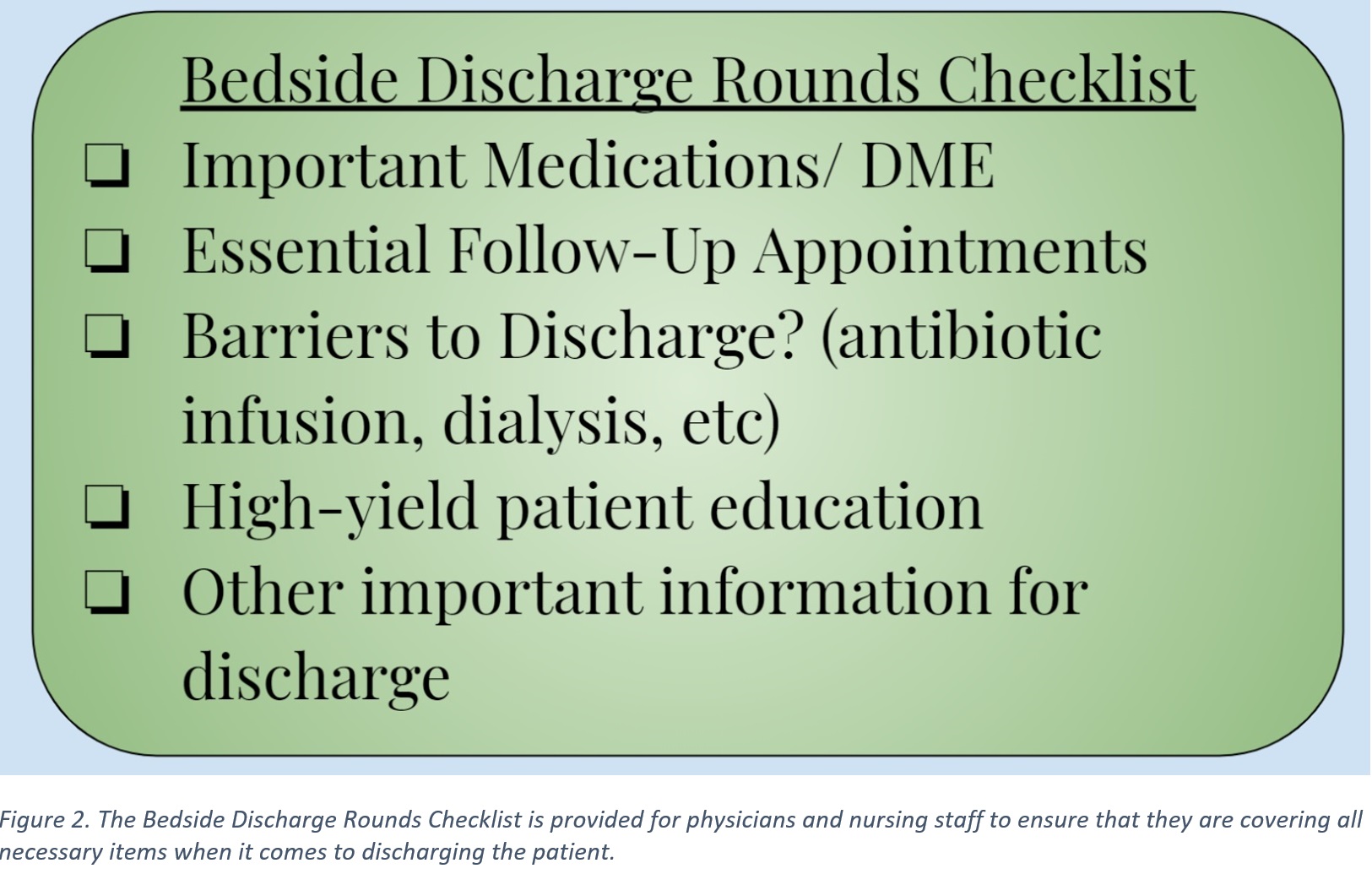
Conclusions: Currently there are gaps in interprofessional communication at the time of discharge providing a clear opportunity for improvement. In our current model, providers have patients assigned throughout the hospital which requires communication with several nurses on different floors and limits face to face interactions. This creates barriers to communicate the discharge plan effectively. From surveys, providers were more comfortable than nurses with the current communication system which involves updating patient information in the EMR with resulting After-Visit Summary. This limits 2-way communication between providers, nurses, and patients, reducing the ability to ask questions or clarifications. Our institution is working towards “geolocalizing” provider-patient assignments which could help eliminate some of these barriers. Following this implementation, the next step will be to introduce a standardized patient-centered discharge process (Figure 1) and checklist (Figure 2). This would include having the provider and nurse at the bedside to discuss the discharge plan together with the patient, ensuring open communication and likely a safer and more effective transition of care. Limitations of this study include single center and the assumption that the current communication model is leading to poor patient outcomes which we plan to study with the change in discharge communication.