Background: The relation of a patient’s age to survival in cardiac arrest is often discussed at the bedside when clinicians, patients, and families are faced with the question of whether CPR is medically appropriate for elderly individuals. Few studies are available to help guide this conversation. This study sought to evaluate in-hospital cardiac arrest (IHCA) outcomes in geriatric patients at our institution.
Methods: This is a retrospective analysis of all patients at a community teaching hospital from 1/2018 to 5/2019 who experienced IHCA with a focus on geriatric patients. The primary outcomes were rate of initial return of spontaneous circulation (iROSC) and rate of survival to discharge (StD). Secondary analyses included presence of initial shockable rhythm or any shockable rhythm, time when initial code occurred, and effect of bicarbonate on obtaining iROSC and StD. Although binary logistic regression was performed for both outcomes, quasi-complete separation of data points limited our StD analysis.
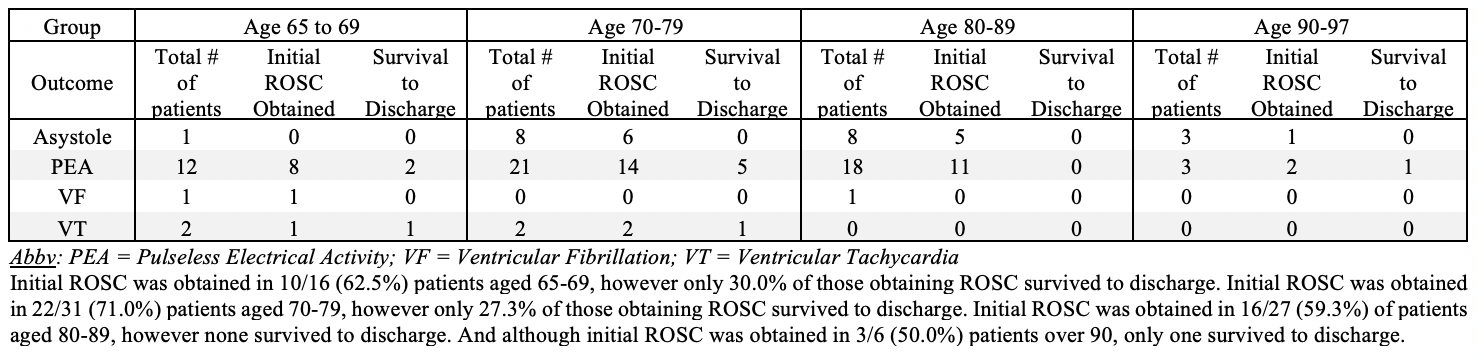
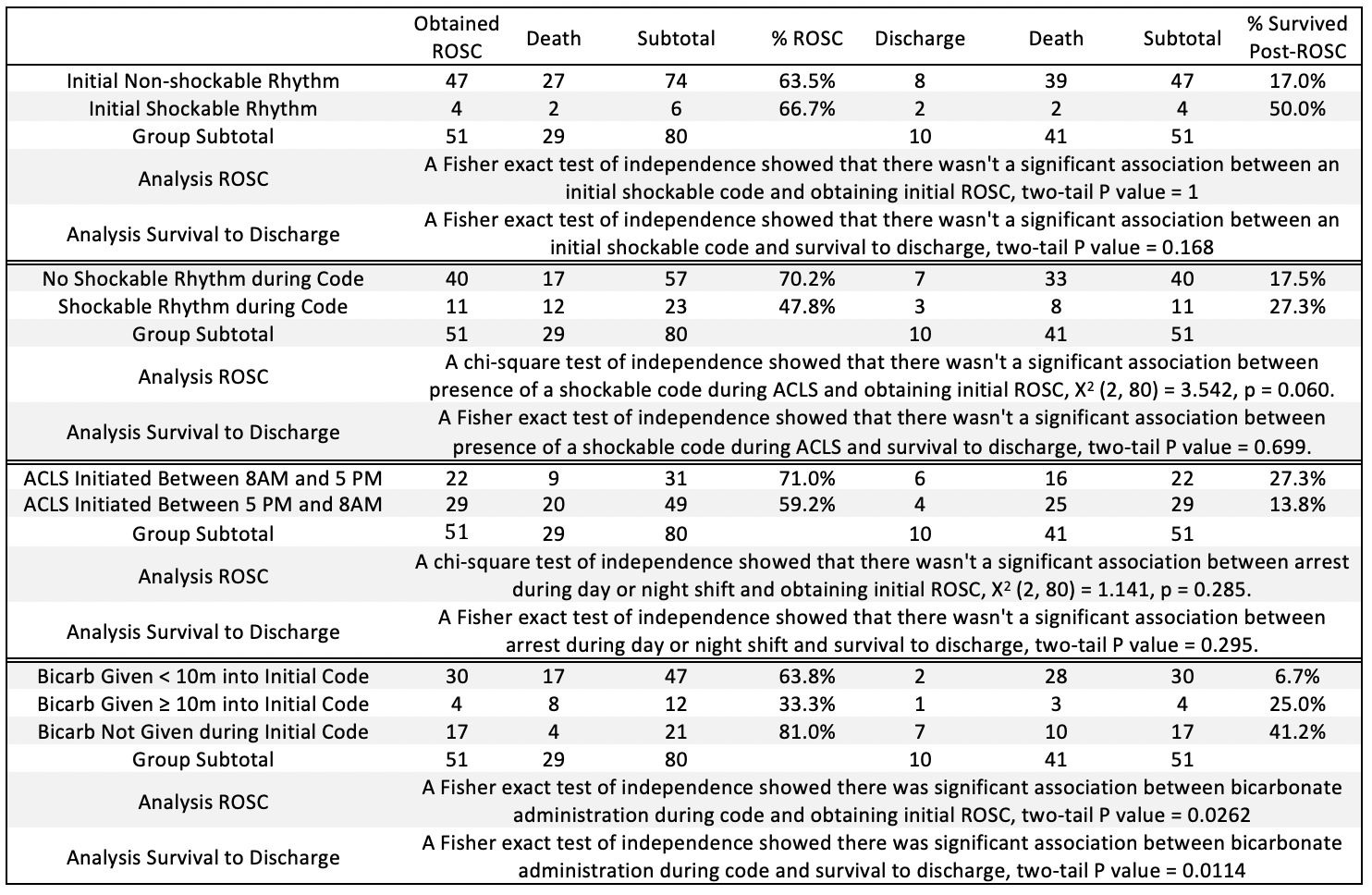
Results: 115 patients experienced 156 IHCAs during this time. 80 patients ≥65 represented 106 of the 156 IHCAs. 30/35 patients <65 obtained iROSC (85.7%), 14 of which reached StD (45.7%). However, 51/80 patients ≥65 obtained iROSC (63.8%), 16 of which reached StD (19.6%). When analyzed by age group (<65 and ≥65), chi-square test of independence showed significant association between age and iROSC [X2 (2, 115) = 5.641, p = 0.0175] as well as StD [X2 (2, 81) = 6.633, p = 0.0100]. Of note, only 19/33 patients ≥80 obtained iROSC, of which 1/19 reached StD (See Table 1). No significant associations were found between initial shockable rhythm, presence of shockable rhythm, or time of code with obtaining iROSC or StD (See Table 2). Although chi-square testing showed there was a significant association between bicarbonate use during the initial code and lower rates of obtaining ROSC, this association was lost when accounting for covariates.
Conclusions: Few studies look at geriatric IHCA outcomes. Our findings support existing literature showing elderly patients tend to have lower crude survival rates than younger patients. Non-shockable rhythms associated with worse outcomes also tend to predominate in this age group, which we observed. However, a recent study found geriatric patients often have good neurological outcomes if they reach StD – even if ≥90. The 92-year-old in this study who reached StD is still alive >1-year post-arrest and ambulatory. Regardless of age, the desired outcome after obtaining ROSC is one where the patient has an acceptable quality of life as they define it. For this reason, code status should continue to be individualized on a case-by-case basis.