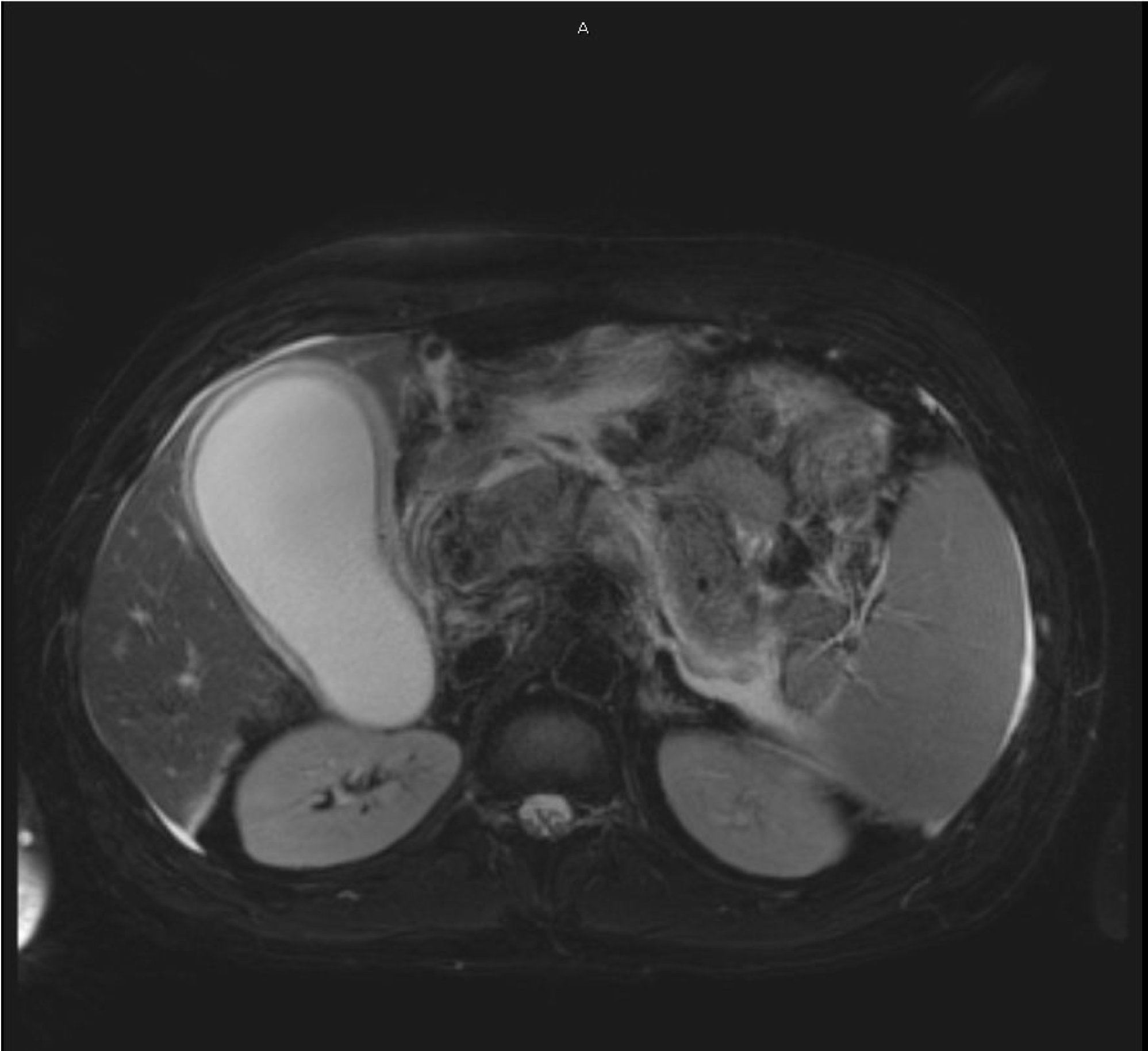
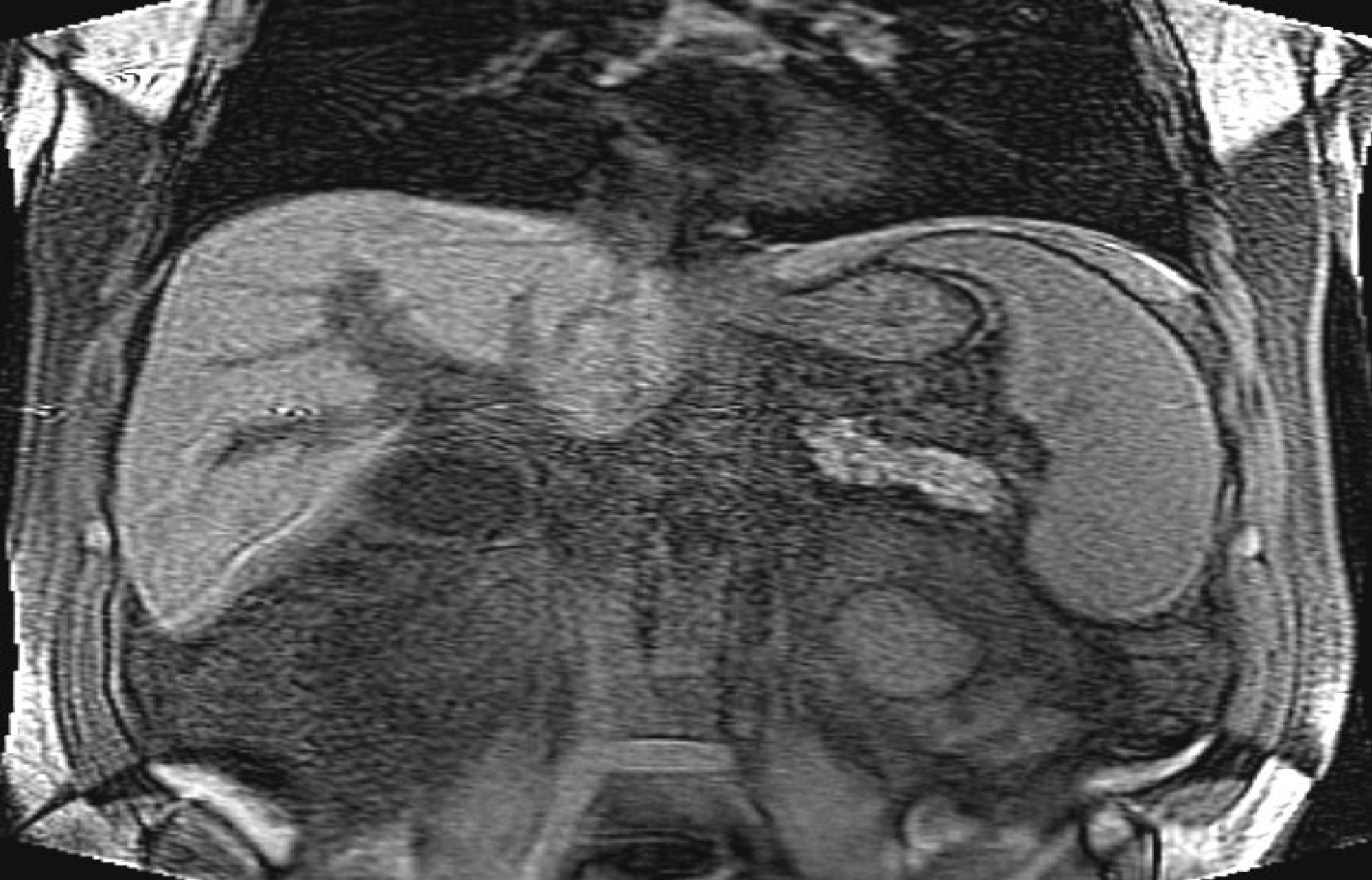
Case Presentation: A 37 year old man with history of alcohol abuse presented to the emergency department for a one month history of jaundice, nausea, vomiting and weight loss. Physical exam was significant for mild diffuse abdominal tenderness and jaundice. Labs were remarkable for a total bilirubin of 34.1, direct 17.5, alkaline phosphatase of 203, AST 45, ALT 37, amylase 32 and a lipase of 3. Imaging studies including ultrasound of abdomen showed hepatomegaly, a CBD diameter 3cm, and intrahepatic biliary duct dilation, but no focal liver lesions. MRCP showed acute pancreatitis and intrahepatic biliary duct dilatation but without clear stricture or obstructing stone. Abdominal MRI showed cavernous transformation of the superior mesenteric vein likely secondary to chronic thrombosis, collateral formation and CBD obstruction secondary to mass effect from hilar varices.The patient underwent ERCP with plastic stent placement. His Jaundice significant improved. Workup for hypercoagulable states including protein C total, protein S antigen, factor V leiden, prothrombin gene mutation 20210A, antithrombin III antigen, JAK2 v617 were negative. Given the chronicity of the mesenteric vein thrombosis and EGD evidence of esophageal varices, the patient was not a good candidate for anticoagulation. He was discharged with close follow up and a plan to remove the plastic stent by gastroenterology in the coming months if there is no more evidence of obstruction.
Discussion: The biliary system is composed of left and right hepatic ducts that join after exiting the liver with the cystic duct draining the gallbladder to become the common bile duct which joins the pancreatic duct before draining it’s contents into the duodenum. This structure is closely followed by the portal vasculature for much of it’s course. The disease process seen in our patient was first described in 1965 when a case of bile duct compression was attributed to varices causing extrinsic compression of the CBD. Portal biliary ductopathy (PBD) involves obstruction of the biliary tree in the setting of portal hypertension due to collateral formation. This portal hypertension is usually secondary to portal vein thrombosis which is idiopathic in up to 50% of patients. Other causes include chronic pancreatitis, myeloproliferative disorders, tumor invasion, intra-abdominal sepsis, and schistosomiasis. The pathophysiology is usually extrahepatic cavernous transformation of the portal vein and compression of the extrahepatic biliary ducts which in turn cause retrograde dilation of the intrahepatic biliary system.The presentation of PBD is variable and includes symptoms such as abdominal pain and jaundice. Prolonged obstruction may lead to secondary liver cirrhosis and liver functional decline. Magnetic resonance cholangio-pancreatography is the recommended first line investigation and ultrasound with color doppler may be used in conjunction to survey surrounding structures and to rule out other pathology such as tumors.
Conclusions: Portal biliary ductopathy is a very rare cause of obstructive jaundice. There is a broad differential diagnosis for Jaundice and our purpose is to educate and promote awareness of PBD. Portal vein thrombosis is the most common cause of PBD. PVT is diagnosed with abdominal imaging including Ultrasound with doppler, CT, and MRCP. Patients should be evaluated for prothrombotic states, liver disease, and malignancy.