Background: Over the last 2 decades there has been increasing adoption of Observation (OBS) units across the healthcare facilities in United States. Health reforms like 2 midnight rule and 30 day readmission penalties, congestion in the ED, poor operational outcomes in OBS population mixed with inpatients (IP) etc. further added to the need for dedicated OBS units.
Purpose: In most Healthcare facilities, OBS units are established in close proximity to the emergency room and often run by Emergency Department. They are classified as Level I OBS units or Clinical Decision Units (CDU) providing protocol based care for specific diagnosis. Patients who do not fit the criteria of CDU but classified as OBS are often admitted to medical-surgical floors under Hospital Medicine or other services.On a retrospective analysis of discharge data of OBS patients on Hospitalist service from Jan 1- Apr 30, we noted that the average OBS length of stay (LOS) for Hospital Medicine service was 55.6 hours. Most of these patients were admitted to random units which was determined by bed availability at the time of admission and lacked geographic clustering of OBS patients. These patients were further assigned to different Hospitalist rounding teams to maintain floor geography of the existing unit and teams. We hypothesized that, geographically clustering OBS patients and providing team-based care would result in improvement in quality of care and outcome metrics in OBS patients.
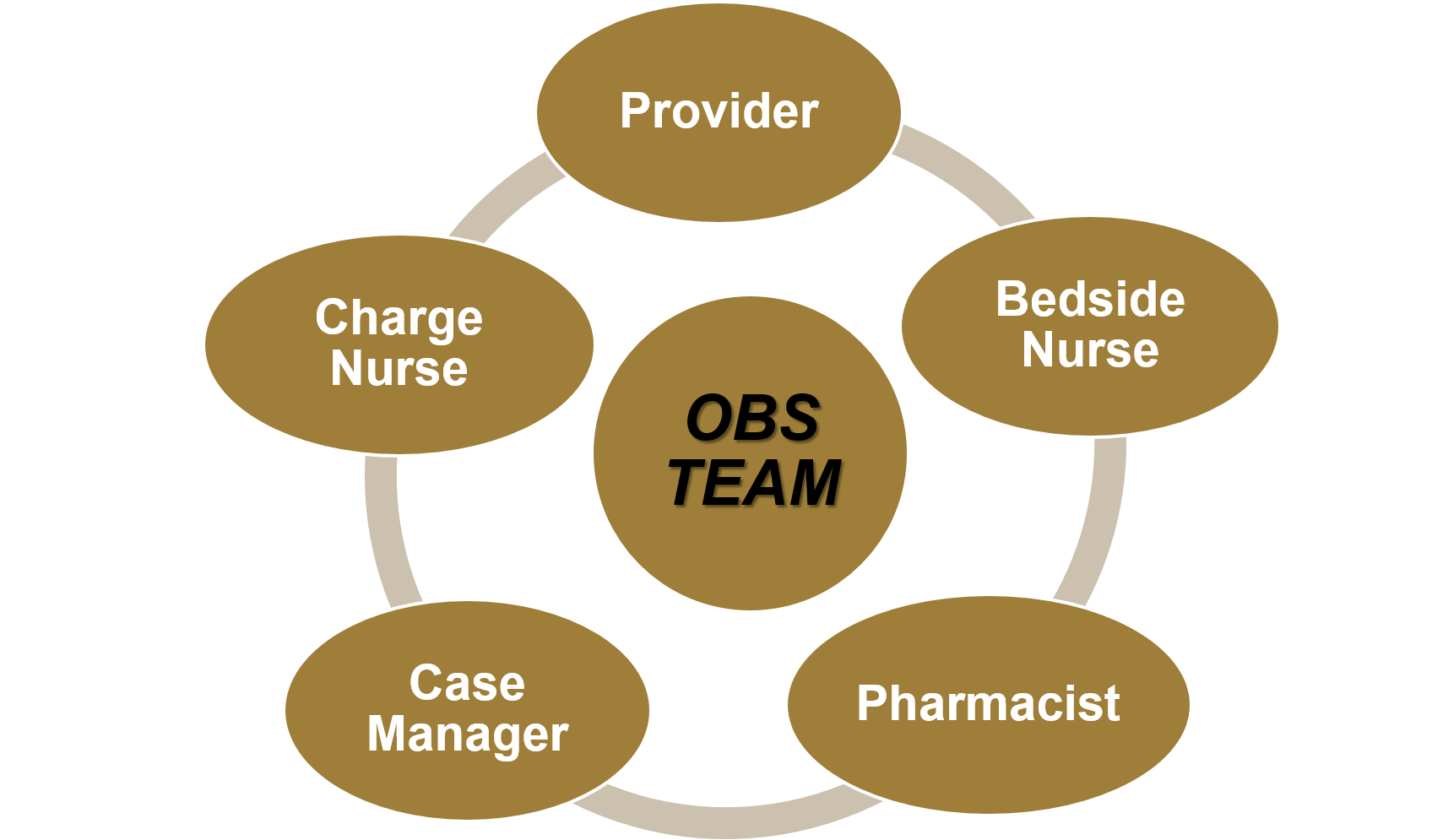
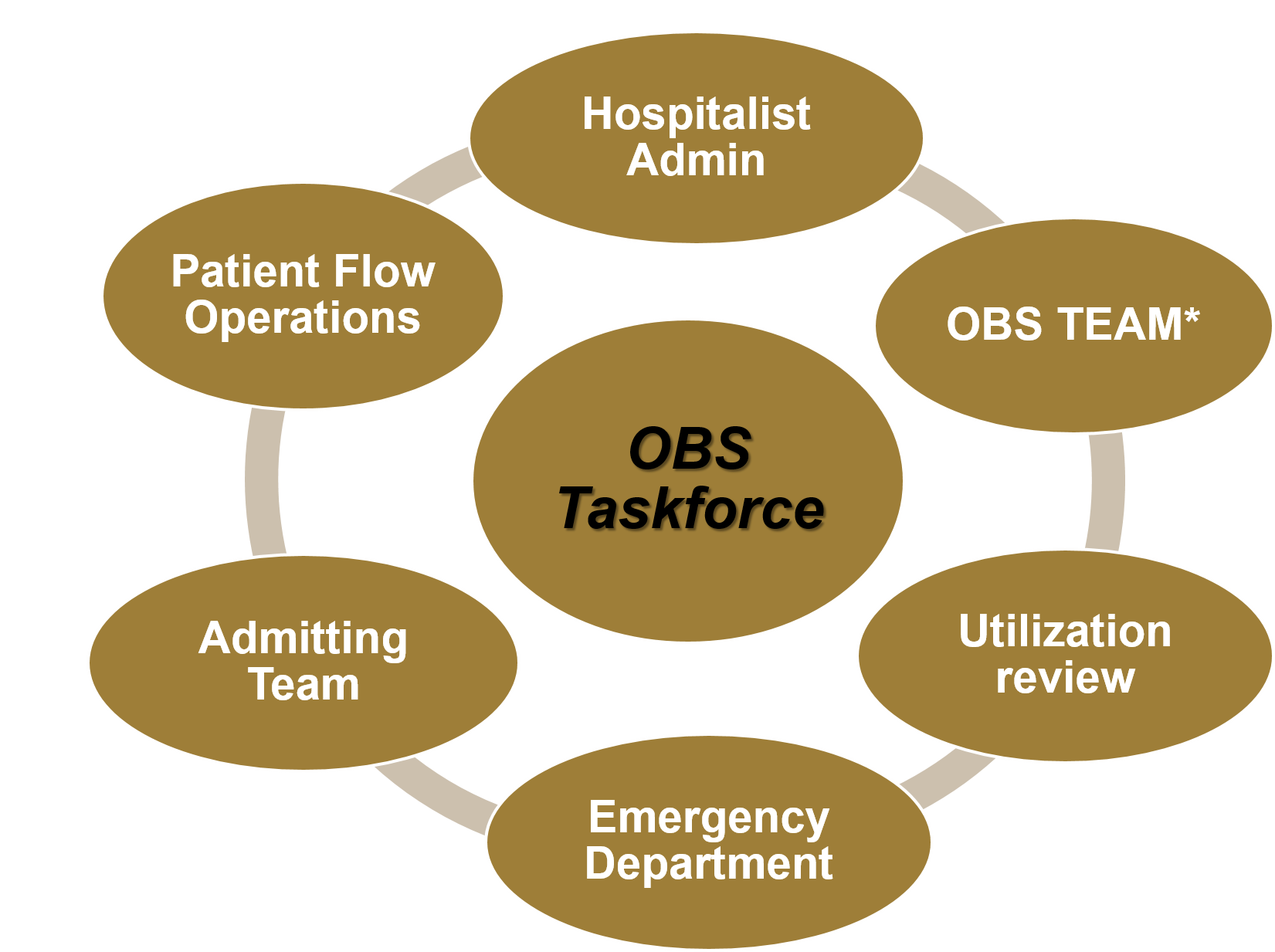
Description: We created a dedicated 14 bed OBS unit on med-surg floor run by Hospital Medicine. ED triage, admitting team, patient flow operation played a vital role in cohorting the OBS patients on OBS unit. We established an OBS team (Figure 1) consisting of Providers, Nursing, Care coordination, Pharmacy who performed conference room huddle every day at 10 AM and 3 PM. Utilization review performed timely and frequent case reviews and informed the team about any changes to patient class. We created OBS taskforce (Figure 2) comprising leaders in areas of Hospital Medicine, Nursing, Pharmacy, Care coordination, Patient Flow Operations and Triage closely monitoring the implementation of OBS unit and streamlining the process.Several metrics related to implementation, process and outcome like patient encounters, staffed beds, patient census, OBS to inpatient conversion rate or admission rate, OBS LOS (hours), discharge count and discharge order to discharge time were tracked to streamline the process. Major initial barriers were related to keeping all 14 beds open due to nursing staffing constraints, communication issues leading to triaging of a non-OBS patient or non-Hospitalist service patient to OBS unit, misjudgment of patient class at the time of admission, poor utilization of the OBS beds. The OBS taskforce met weekly for first 6 weeks of implementation period followed by biweekly after that (once the process stabilized) to address these barriers.
Conclusions: With the help of OBS taskforce and OBS team we were able to successfully establish a 14-bed Level II OBS unit in a large academic center. Within 5 months of implementation, OBS unit saved 371.5 bed days. Emphasis on team based care, geography and developing a distinctive mindset pertaining to care delivery of OBS patients played a crucial role in laying foundation for a robust OBS unit.