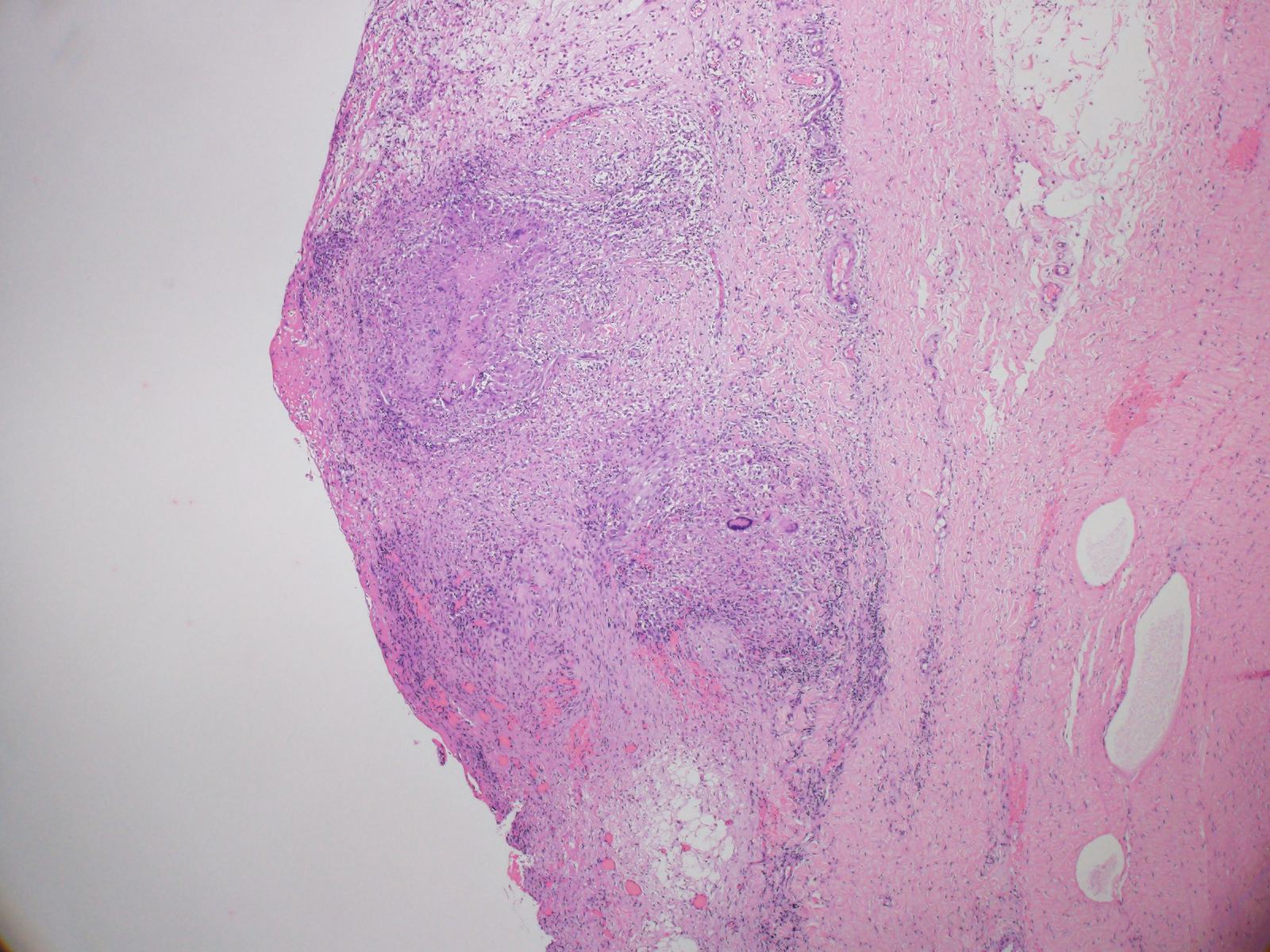
Case Presentation: A 47-year-old previously healthy male was referred from another hospital with fever, dry cough, abdominal pain and diarrhea for about one month. He also had unintentional weight loss of 33 lbs and abdominal distention over 2 months. He was originally from Nigeria and had moved to Japan 10 years ago. A physical exam was notable for abdominal distention with diffuse tenderness to palpation and rebound. His white blood cell count was 4.1 K/μL. CT of the chest, abdomen and pelvis revealed large ascites with a thickened peritoneum and prominent mesenteric lymph nodes. Ascites fluid analysis showed >1,483 leukocytes (10% neutrophils, 85% lymphocytes, 5% macrophages) and elevation of adenosine deaminase to 128 IU/L. Fluid cytology was negative for malignancy. Serology for HIV was negative, but a tuberculosis IGRA test was positive. All smear, PCR, and culture tests for tuberculosis from sputum and ascites fluid were negative. Esophagogastroduodenoscopy and colonoscopy were unremarkable. At this point, peritoneal tuberculosis was a major concern. After discussion with consultants, exploratory laparoscopy was performed, and demonstrated innumerable white, miliary nodules on the peritoneum and omentum (Image 1). Specimens of parietal peritoneum were obtained on biopsy, and histopathological analysis showed caseating granulomas with Langhans giant cells (Image 2). The patient was started on empiric treatment with isoniazid, rifampin, pyrazinamide, and ethambutol. Subsequently, a culture from the peritoneum grew Mycobacterium tuberculosis that showed resistance to both isoniazid and rifampin. The patient was transferred to a research hospital to start treatment for multidrug-resistant tuberculosis.
Discussion: The reported incidence of peritoneal tuberculosis (PTB) among all forms of tuberculosis is only 0.1 to 0.7%. As well as being rare, diagnosis of PTB is challenging because of its nonspecific clinical features that overlap with conditions such as liver cirrhosis, malignancy, and autoimmune diseases. Intensive work up is often necessary to confirm or exclude other potential diagnoses. Analysis of ascites fluid for markers such as SAAG, CA-125, and ADA can support diagnosis of PTB, but this is not conclusive. AFB smear and culture from ascites fluid are rarely helpful due to low sensitivities of up to 3% and 21-35% respectively. Ultimately, if the diagnosis is uncertain, laparoscopic examination with peritoneal biopsy and subsequent pathological or microbiologic confirmation should be considered, since this can have a sensitivity of 93%. Obtaining susceptibility culture results from biopsy is also important, especially for a patient from a region with a high rate of drug-resistant tuberculosis. Our patient was from Nigeria, where tuberculosis is endemic and the prevalence rate of drug resistance among new tuberculosis cases is as high as 32.0%. Careful attention to the background of the patient in our case avoided misdiagnosis and led to appropriate treatment for multidrug-resistant tuberculosis.
Conclusions: This rare case of peritoneal tuberculosis highlights the importance of obtaining tissue for diagnosis and culture susceptibility tests. Drug-resistant pathogens such as multidrug-resistant Mycobacterium tuberculosis are more widespread than ever, and clinicians should pay attention to the background of the patient in cases that may involve such pathogens.