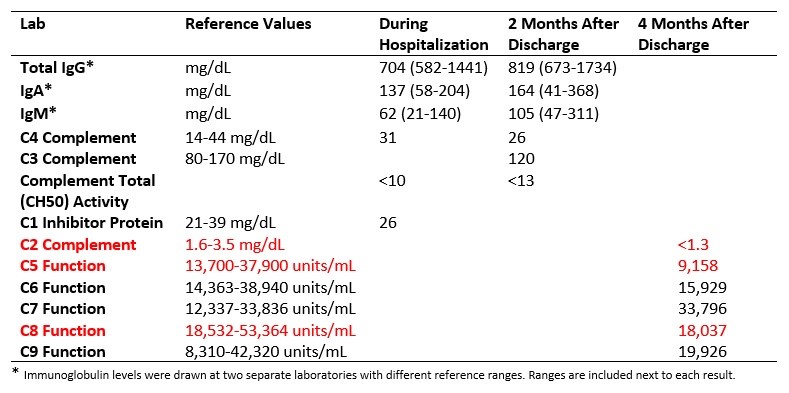
Case Presentation: An otherwise healthy 9-year-old, fully vaccinated, male initially presented to urgent care with acute onset of sore throat, fever, trouble swallowing, and mild intermittent dyspnea. Due to worsening respiratory distress the patient was brought to an emergency department where he was found to have hoarse voice, trismus and in sniffing position. Laboratory testing was significant for leukocytosis with left shift and elevated inflammatory markers. Stridor on respiratory exam was concerning for upper airway obstruction. An X-ray of the neck showed thickening of the epiglottis, consistent with epiglottitis. He received methylprednisolone, ceftriaxone and vancomycin for presumed epiglottis. Blood cultures grew Haemophilus influenzae at 48 hours. Further history revealed GBS meningitis at 6 days of age, two episodes of acute otitis media and first episode of epiglottitis 3 years ago. He had received all his immunizations and had otherwise been healthy, with normal growth and development. Due to his bacteremia, recurrent epiglottitis and history of GBS meningitis, an immunodeficiency evaluation was initiated. Initial labs showed normal immunoglobulin levels and normal levels of complement factors C3 and C4. However, the patient had abnormal CH50 activity, < 10 and < 13 on repeat (normal: 31 - 60 U/mL). Titers for Hib (Haemophilus influenzae type B) IgG were indeterminate, and he only demonstrated adequate levels in 2 out of 13 PCV (Pneumococcal conjugate vaccine) serotypes despite being fully immunized. Further immunological studies revealed C2 factor level less than the limit of detection (Table 1). His Hib vaccine series, PCV 13, PCV 23, and Meningococcal conjugated vaccine were repeated after hospital discharge.
Discussion: A thorough history-taking is crucial in the diagnosis of this patient’s underlying immunodeficiency given that patient has been a normally growing, normally developing, and perceived to be a relatively healthy boy. Prevalence of primary immunodeficiency in children is about 1 in 2,000. Initial immunological work up with normal immunoglobulin levels made humoral deficiency less likely in this patient. His C3 and C4 level were normal, but his complement activity, measured by CH50, was significantly low indicating a problem within his complement cascade. Complement deficiencies are rare and make up less than 10% of primary immunodeficiencies, with the most frequently affected factor being C2. The complement arm of the innate immune system is responsible for opsonization, phagocytosis and activation of the inflammatory response. Those with classical pathway component deficiencies, which includes C2, tend to have infections with encapsulated bacteria such as S. pneumoniae, H. influenzae and N. meningitidis.
Conclusions: Recurrent serious bacterial infections should prompt pediatricians to assess the patient’s immune system. Not all immunodeficiencies present early in childhood with frequent invasive infections. Having recurrent epiglottis is especially rare, making it one of the components of our patient’s history which was quite unusual, leading the medical team to evaluate for immune deficiency.