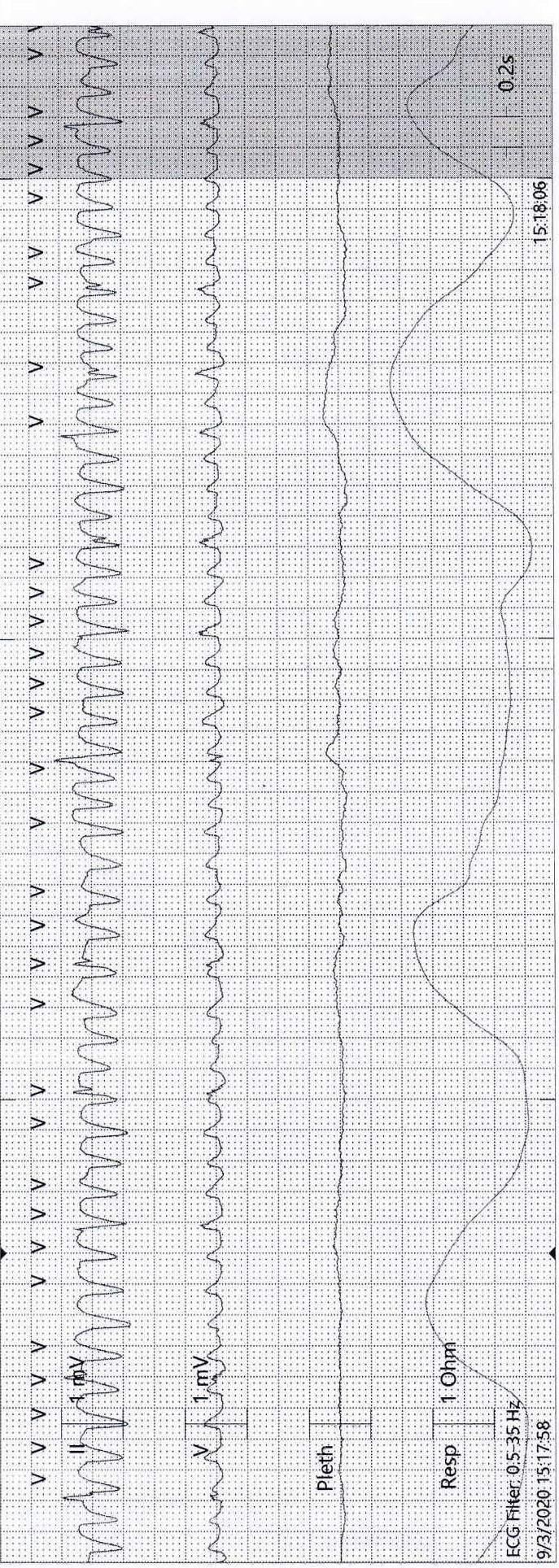
Case Presentation: Our patient is a 90-year-old Caucasian female with atrial fibrillation, peripheral vascular disease, and hypertension was admitted to the hospital due to shortness of breath for one day and myalgias for the past three days. Her chest x-ray done on presentation was consistent with multifocal pneumonia, and on further testing, she was subsequently diagnosed with COVID-19. During the hospital course, the patient started having intermittent episodes of sustained wide complex tachycardia with heart rate (HR) noted to be in the 190s beats per minute (bpm) on cardiac monitor, concerning for ventricular tachycardia(VT). She was clinically asymptomatic, on physical examination the patient was hemodynamically stable with HR in 80’s, and blood pressure of 126/64, and oxygen saturation in the low 90’s on 2 liters of supplemental oxygen. A 12 lead ECG done showed atrial fibrillation with HR of 72 bpm. Laboratory workup including serum potassium, magnesium, troponin, and brain natriuretic peptide (BNP) were all within normal limits. She was started on oral metoprolol tartrate 12.5 mg twice daily. A transthoracic echocardiogram could not be done due to her COVID status. She did not have any further episodes of VT on telemetry. However, on further analysis of the telemetry strip, hidden narrow-complex beats were identified throughout the rhythm strip and the intermittent wide complex tachycardia identified earlier was labeled as an ECG artifact. The patient didn’t have any recurrence of arrhythmias and later passed away from COVID pneumonia complication.
Discussion: ECG artifacts are defined as ECG aberrancies, which result from the measurement of potentials generated on the body surface and are not related to the electrical activity of the heart [1]. ECG artifacts may arise due to both internal (physiological) such as tremors and external (nonphysiological) sources such as a loose lead [2]. Most often artifacts in ECG are recognized as incorrect signals not impacting ECG interpretation, however, some signals mimic disease patterns and may present a challenge to physicians to tell them apart. In patients with significant coronary heart disease (CHD) or other structural heart diseases, a wide QRS complex tachycardia (WCT) should be considered to be ventricular tachycardia until proven otherwise. However, consider an ECG finding as an artifact, when observed on a rhythm strip in a patient who remains asymptomatic and hemodynamically stable. In our case, the patient’s movements while eating caused a motion artifact. An artifact is highly likely if narrow-complex beats can be identified regularly “marching” through the rhythm strip, as was seen with our patient. One-to-one association between P waves and QRS complexes excludes wide complex tachycardia.
Conclusions: The presence of ECG artifacts may lead to unnecessary non-invasive and invasive interventions [3]. Therefore early recognition of ECG motion artifacts masquerading as serious diseases such as ventricular tachycardia is important to avoid raising a false alarm and help prevent such unnecessary consequences. Interpretation of a rhythm strip, particularly in correlation with the clinical presentation of the patient as well as pertinent cardiac history may help early recognition of ECG artifacts and should always be practiced whenever faced with a suspicious rhythm or a contradicting clinical vignette.