Case Presentation: A 61-year-old male with biopsy-proven untreated pulmonary sarcoidosis presented with altered mental status and fever. He had recent admissions for occipital CVA after presenting with dizziness and blurred vision, and pulmonary emboli after presenting with fevers and dyspnea. Urinalysis and blood cultures were negative. (1-3)-B-d-glucan was elevated to 246 pg/mL (<80pg/mL). Urine Histoplasma and Blastomyces antigens were negative and fungal serologies were sent. PET/CT showed a hypermetabolic lung (favored to represent infarct vs. malignancy) and bilateral adrenal nodules. Fever and dyspnea resolved with anticoagulation and lung biopsy was planned after repeat imaging. Upon current presentation, he was febrile and disoriented with a new CN III deficit. MRI/MRA brain showed new infarcts in multiple vascular territories with leptomeningeal enhancement. (1-3)-B-d-glucan remained elevated. Prior fungal serology remained pending. Repeat urine fungal studies were negative. CSF studies showed elevated RBCs, WBCs with neutrophilic predominance, elevated protein, and low glucose. During admission, he developed a new CN VI palsy, myoclonus and rapidly progressive lethargy. Empiric amphotericin was initiated with resolution of fevers and neurologic improvement.After treatment initiation, Histoplasma fungal serology, immunodiffusion (H and M bands), serum antigen and CSF antibodies returned positive. He was treated with a 6-week course of amphotericin, transitioned to voriconazole indefinitely, and discharged home with near complete resolution of symptoms.
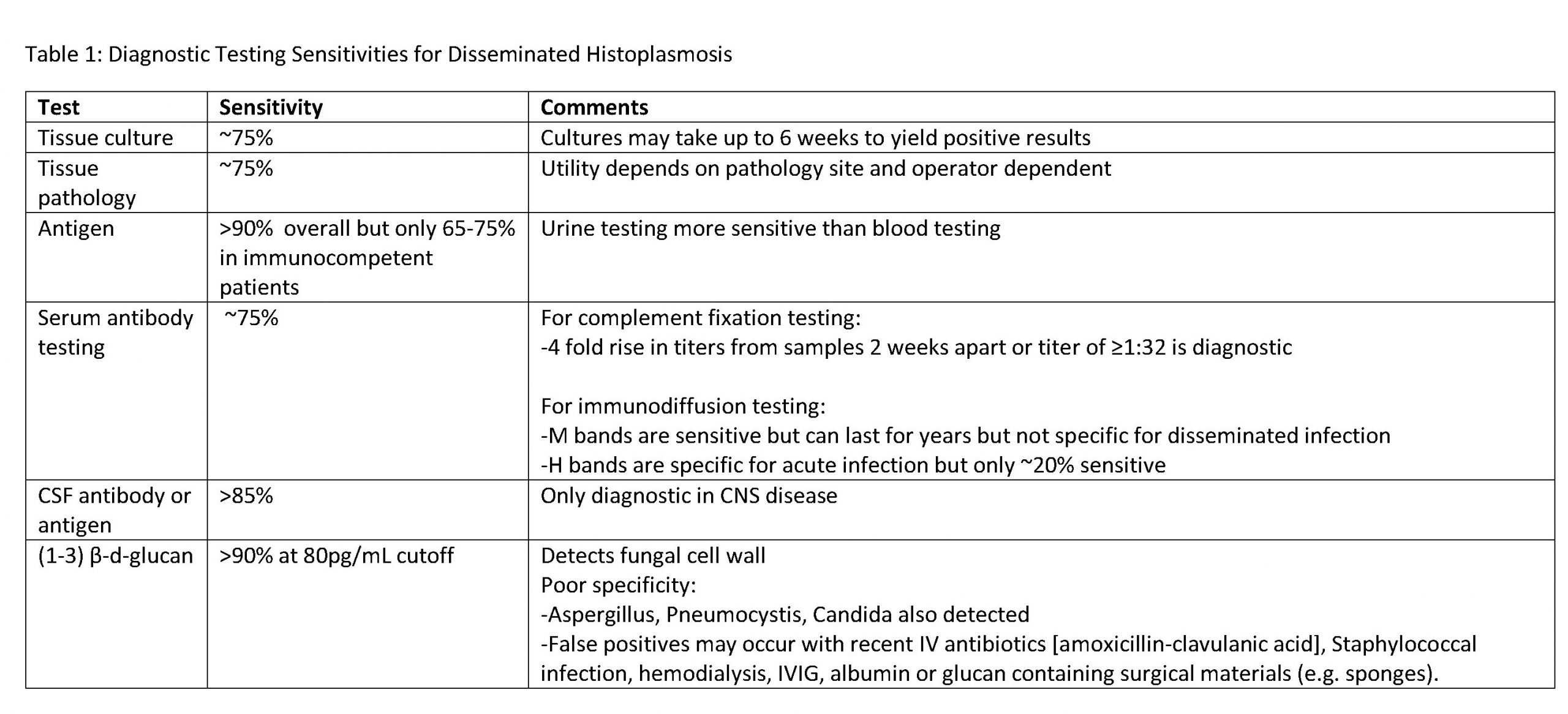
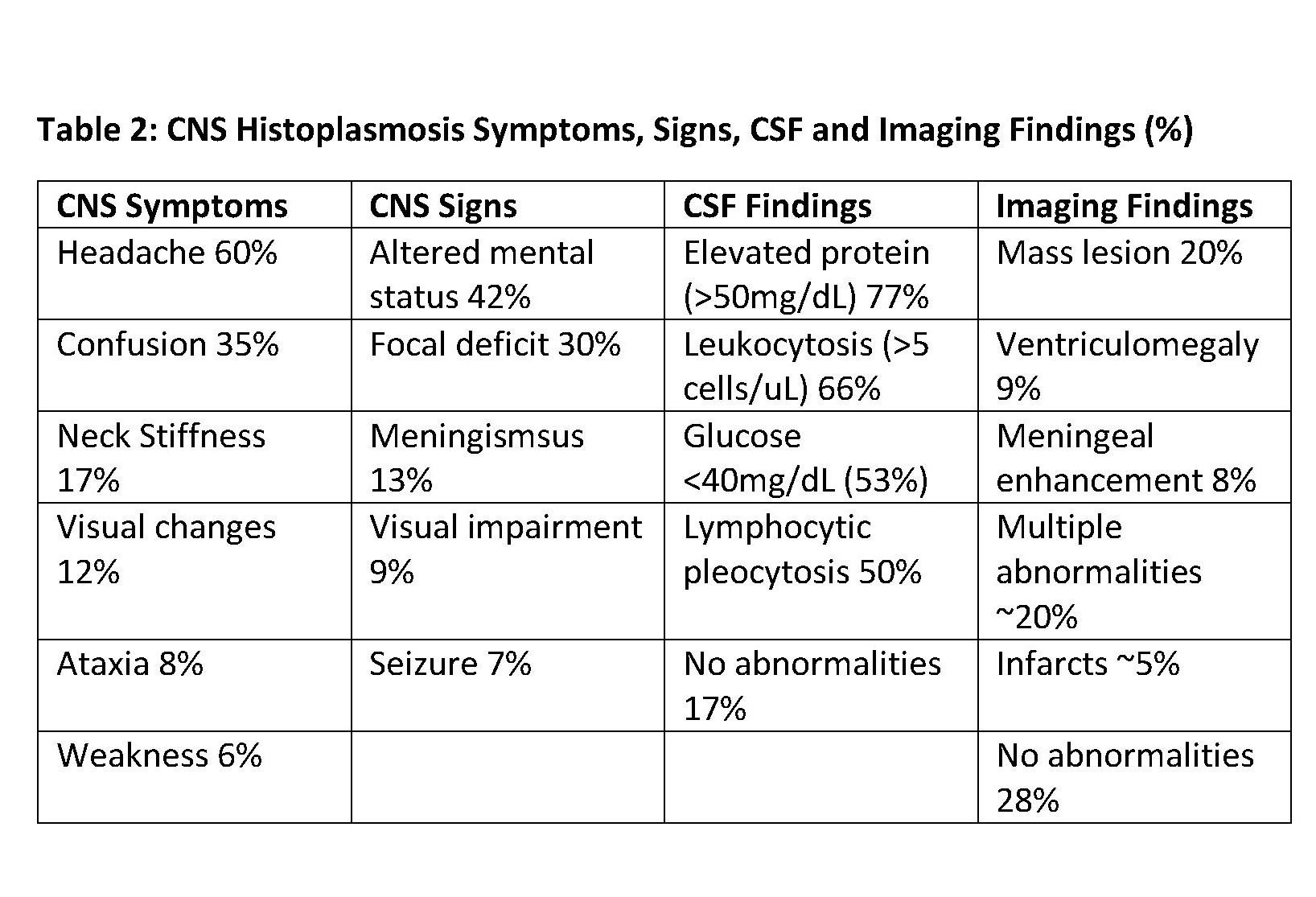
Discussion: Disseminated (i.e. extrapulmonary) histoplasmosis occurs in ~1/2000 patients with acute infection with most infections occurring in the upper Midwest. Risk factors for disseminated disease include age extremes (infants or >65 years), immunocompromise (AIDS, organ transplant, use of corticosteroids or TNF-a inhibitors), and other T-cell disorders. Nearly all organs may be involved in disseminated disease, but clinically silent involvement of the GI tract (~70%) and adrenal glands (>80%) are common. CNS disease occurs in 5-20% of patients with disseminated disease. Diagnosing CNS histoplasmosis is challenging because of its nonspecific presentation. Symptoms, signs, CSF findings, and imaging are summarized in Table 1. Most diagnoses (~60%) are delayed by >1 month with early mortality of 20-40%. Misdiagnosis as neurosarcoidosis, TB or other CNS infection, inflammatory disease, or malignancy is common. Test characteristics for disseminated histoplasmosis are crucial to diagnosis (Table 2). Notably, urine antigen is only 65-75% sensitive for disseminated histoplasmosis in immunocompetent patients, while (1-3)-B-d-glucan has very good sensitivity but limited specificity.
Conclusions: In this case, an immunocompetent patient with sarcoidosis was diagnosed with CNS histoplasmosis. Diagnosis was challenging due to the overlap in clinical presentation between these diseases. Sarcoidosis is associated with dysfunctional Treg cell subpopulations which has been theorized to increase the risk of disseminated Histoplasma infection, and many patients with sarcoidosis are iatrogenically immunosuppressed, increasing their risk of disseminated disease. Understanding the diagnostic test characteristics for histoplasmosis, the overlap with sarcoidosis, and multidisciplinary discussions ultimately spared this patient significant morbidity from anchoring bias on an existing diagnosis.