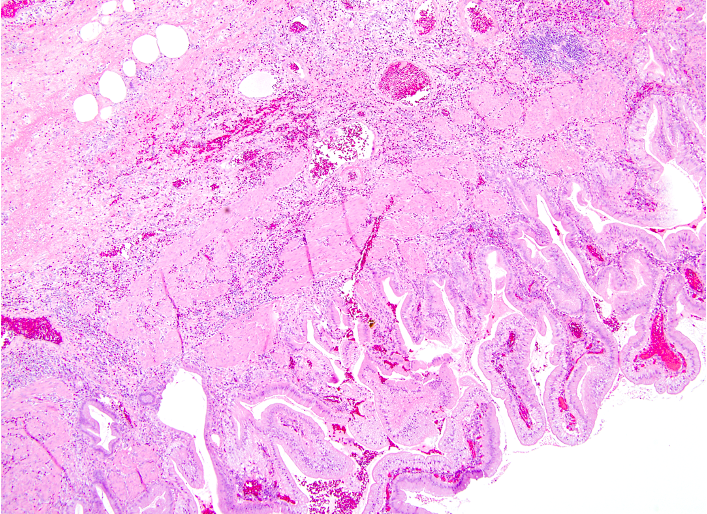
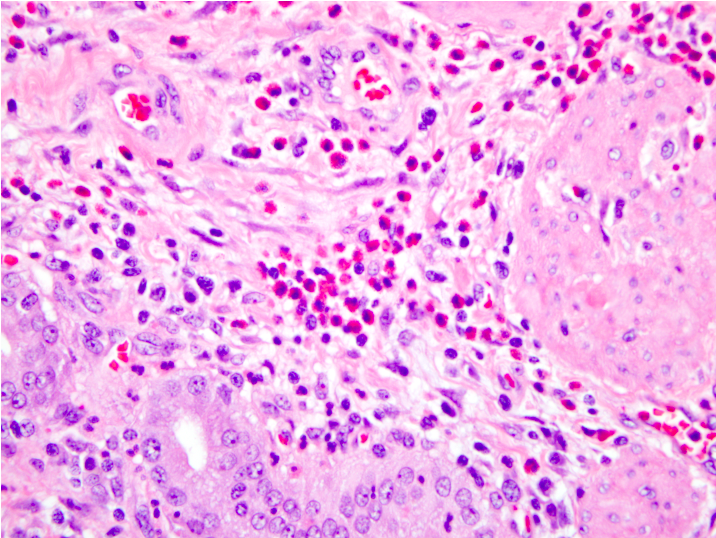
Case Presentation: A 60 year-old male presented with 2 weeks of abdominal pain, anorexia, and constipation. His abdominal pain was crampy, generalized, and progressively worsening in severity. His medical history was significant for alcohol abuse and gallstone pancreatitis. He was abstinent from alcohol for the 2 days preceding presentation secondary to “not feeling well.” He was afebrile with normal vital signs. He had mild epigastric tenderness to palpation and abdominal distension. Labs showed a leukocytosis of 13.6 x109/L with neutrophilic predominance, eosinophilia (0.8 x109/L), elevated aspartate aminotransferase (56 U/L), hyperbilirubinemia (total 2.1 mg/dL), elevated lipase (2,511 U/L), and a baseline elevated creatinine of 1.8 mg/dL. Notable normal labs included alanine aminotransferase, alkaline phosphate, and serum triglycerides. Computerized tomography scan of the abdomen/pelvis showed inflammatory stranding and edema surrounding the pancreas, consistent with acute interstitial pancreatitis. Abdominal ultrasound (US) showed only cholelithiasis. He was started on empiric ceftriaxone and metronidazole at admission. On day 2 of hospitalization, he developed septic shock requiring transfer to the intensive care unit, broadening of antibiotic coverage, and initiation of vasopressors. His total bilirubin increased to 5.6 mg/dL (direct of 4.5 mg/dL) with otherwise stable hepatic function labs. ERCP with sphincterotomy showed sludge, but no stone. Repeat abdominal US showed a distended gallbladder with multiple mobile internal stones, a thickened wall, and pericholecystic fluid. He underwent laparoscopic cholecystectomy without complications and clinically improved to discharge. Pathology of his gallbladder showed thickening of the gallbladder wall secondary to muscular hypertrophy and fibrosis with a prominent eosinophilic infiltrate consistent with eosinophilic cholecystitis (EC).
Discussion: The general internist should be familiar with EC as a distinct disease entity, as it may warrant further investigation into treatable underlying conditions. EC is a rare condition first described in 1949. The clinical presentation is similar to typical cholecystitis, often with right upper quadrant pain and positive Murphy’s sign. Diagnosis of EC is confirmed by histologic analysis of the resected gallbladder showing dense transmural infiltration of eosinophils composing 90% or more of the leukocytes. The etiology is not well understood, but possible causes include allergies, parasites, acalculous cholecystitis, hypereosinophilic syndrome (HES), and eosinophilic gastroenteritis. The diagnosis is important because further work up may be warranted to rule out one of these underlying treatable conditions. In particular, EC with peripheral eosinophilia has been associated with eosinophilic infiltration of other organs, thus a high index of suspicion for eosinophilic gastroenteritis or HES must be maintained. Definitive treatment of EC consists of surgical removal of the diseased gallbladder.
Conclusions: This case presents a rare cause (eosinophilic infiltration) of a relatively common condition (cholecystitis). The general internist should be familiar with EC as it may suggest the presence of another treatable underlying condition, such as an allergy, parasitic infection, or primary eosinophilic disorder.