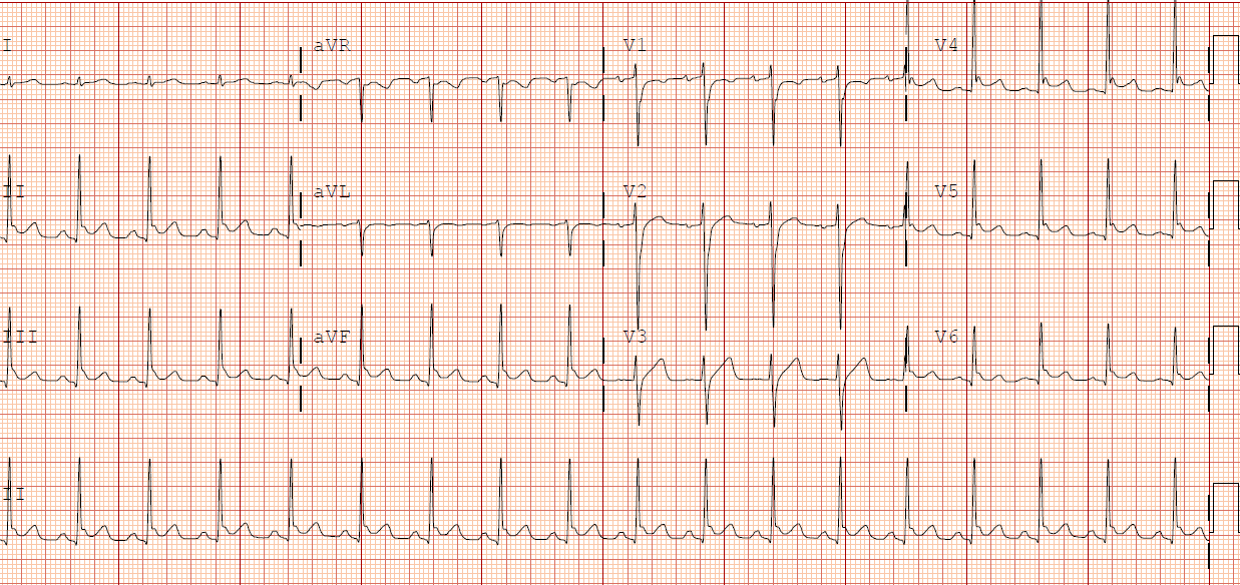
Case Presentation: JD is a 23 yo AA M with no prior PMH presented with fevers, rash, myalgias, chills, nausea and vomiting. The rash began three days prior to admission, began over the palms and spread to the forearms, chest and back. A couple of weeks ago, JD started selling his plasma, prior to that he was an afterschool tutor. No pertinent sexual history and is an occasional smoker. Physical exam pertinent for upper lip swelling, tender lymphadenopathy along anterior and posterior chains and a macular, erythematous rash with coalescence over wrists and palms. Labs pertinent for a mild transaminitis and mild hyponatremia. Microbiology pertinent for positive COVID-19 PCR. On the second day of admission, JD began to have severe chest pain, some difficulty breathing and abdominal pain. The patient became hypotensive to SBP of 70s with minimal fluid response. Labs pertinent for leukocytosis greater than 40,000, BNP of 668, troponin of 0.14, CRP of 216, D-dimer that peaked at 7000, high procalcitonin. EKG with diffuse ST elevations indicative of pericarditis. The patient was started on Ibuprofen, levophed, broad spectrum antibiotics, Remdesevir and Dexamethasone. Transthoracic Echo showed EF of 20% with severe global hypokinesis of the left ventricle and trace pericardial effusion. SCVO2 indicative of cardiogenic shock and dobutamine was added. JD also developed an AKI and coagulopathy. He had gradual recovery and came off of pressors and was ultimately transferred to the floor. HF goal directed medical therapy was initiated and JD was discharged with 4 weeks of Eliquis. Three days later, the JD presented with severe pedal neuropathy with inability to bear weight. MRI spine showed thickening and enhancement of the bilateral lower cauda equina nerve roots, particularly at the L4/L5 levels, consistent with a post-infectious polyneuropathy. Gabapentin was initiated with gradual recovery.
Discussion: Over the course of 2020, we have been continuously learning about COVID management and long-term complications. COVID-associated multi-inflammatory syndrome (MIS) was initially thought to be isolated to children under the age of 21, but there are now almost thirty case reports of COVID-associated MIS in adults. The most common extrapulmonary involvement seen is cardiac, although patients can also have GI, dermatologic, and neurologic complications as seen in our patient. Pathogenesis of MIS remains unclear, but high inflammatory markers suggest the possibility of a disordered immune response. Most cases reported have been in people of color, although there have been no RCTs to assess its true epidemiology. Our patient did not report any family members with similar symptomatology. Although there is no strong evidence on the treatment of MIS, it is commonly treated with steroids.
Conclusions: We describe a rare case of COVID-associated MIS-like syndrome presenting in an adult patient. Internists should be aware that this syndrome may not be limited to patients under the age of 21 and that minority communities may be at elevated risk. In this particular case, we treated the patient with Remdesevir and Dexamethasone with long-term use of gabapentin.