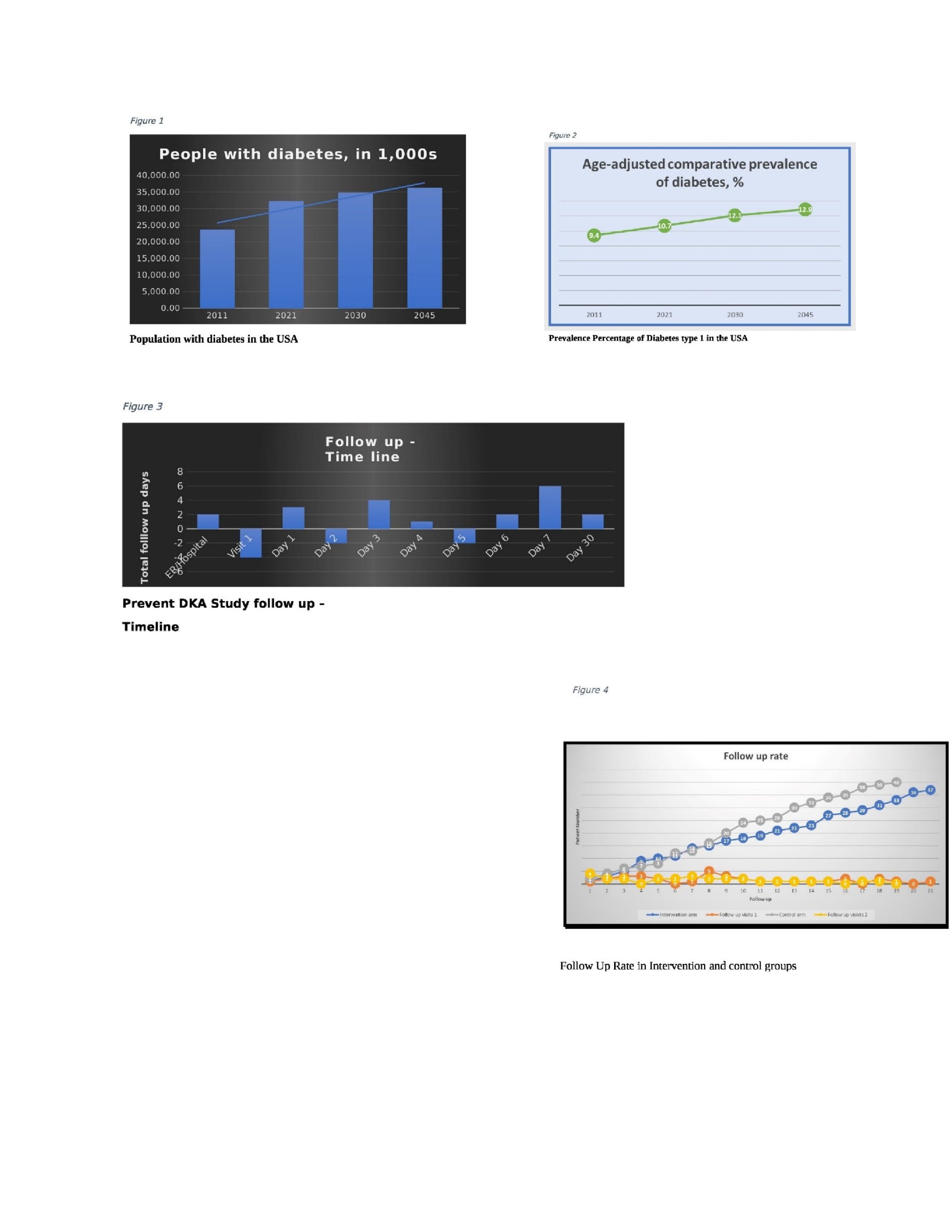
Background: Diabetes mellitus (DM) is a chronic disease where treatment is directed toward reducing and delaying its potentially severe short- and long-term complications. The estimated population (20-79 years old) with diabetes is 32.22 million in the United States, and 12.5% of people live with undiagnosed diabetes (Figure 1). Diabetes Mellitus is currently the most prevalent chronic disease among all visitors to the emergency department. Age-adjusted comparative prevalence percentage has increased by 1.3 % in the US in one decade (Figure 2). Hyperglycemic emergencies, including diabetic ketoacidosis (DKA), are life-threatening medical emergencies that can recur due to a myriad of reasons such as fragmented transitions of care, a lack of availability of insulin, inadequate insulin dosage, or incorrect method of administration. The thirty-day unplanned readmission rate for hospitalized patients with DKA is 19.4%, (1)much higher than the rate for all hospitalized patients. It poses a substantial financial burden to healthcare, and a recent survey indicates a total diabetes-related healthcare expenditure of about 379,470 USD million. Patients are usually advised to follow up with a primary care provider or endocrinologist after their discharge from the hospital, which may take 1 – 2 weeks. While waiting for the next appointment, the patient has to combat diabetes alone (2), and the transition of care is crucial for these patients (3). In this study, we obtained improved results with reduced readmissions due to the intervention of close follow-up during the transition of care from hospital to home and after discharge.
Methods: A single-centered observational prospective randomized controlled trial. We provided intervention through a telephone follow-up as a transition of care from hospital to home after discharge from the hospital for one month. The primary and secondary outcomes are reducing the unplanned return to the hospital and ED/urgent care visits and improved follow-up rates.
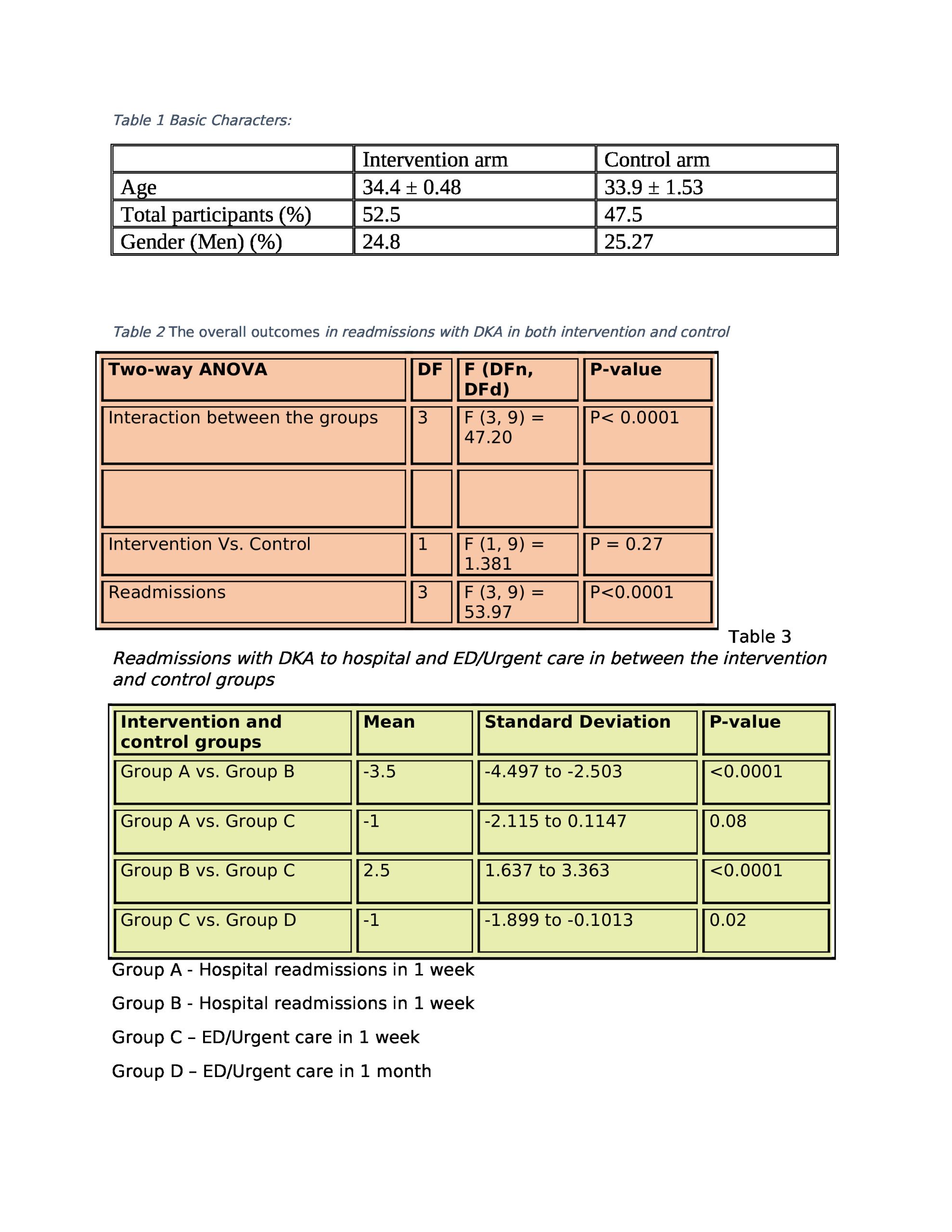
Results: Out of 120 patients screened, 40 were recruited into the study. The mean age was 34, and 25 were men. A reduction in the readmissions to hospital and emergency/urgent care (F (3, 9) = 47.20, p < 0.0001) was observed in both the intervention and control groups of this study. Follow-up after discharge from the hospital showed a significant decrease in the number of readmissions to the hospital compared to emergency/urgent care readmissions (M = 3.5, SD=2.51 – 4. 49, P<.0001) in one week and a reduction in readmissions to hospital compared to ER/urgent care in one month (M=1.5, SD = 0.76-2.24, P< 0.0001) observed with the intervention of contemporary technologies in this study. The follow-up rate to the diabetic clinic was prominently improved in both groups, with a rate of 1.15 and 1.1 with telephone follow-up of this trial.
Conclusions: Follow-up with contemporary technologies decreased the number of readmissions to the hospital due to DKA after initial hospital admission and decreased unplanned emergency/urgent care visits. The improved results show the feasibility of a larger trial and suggest the potential to reduce post-discharge DKA re-admissions and prevent type I diabetes complications.