Background: Hyperthyroidism is a recognized risk factor for atrial fibrillation(AFib). Consequently, current recommendations include screening patients with new onset AFib for thyroid dysfunction by analyzing TSH, T3, and T4 levels. However, the yield of routine testing of patients hospitalized with Afib is less certain. In this study, we evaluated the testing and prevalence of thyroid dysfunction in hospitalized patients who presented with AFib with rapid ventricular rate(RVR). In addition, we strove to further elucidate the underlying risk factors that may be found in those with abnormal thyroid levels.
Methods: Using HCA Healthcare’s clinical data warehouse of 186 hospitals in the US, we performed a retrospective observational cohort study of patients who were 18 years or older from January 1, 2018 to December 31, 2021 and admitted with a diagnosis of Afib and heart rate greater than 110 bpm within the first day of admission. We excluded patients with missing demographics, non-elevated heart rate, or patients already taking methimazole, propylthiouracil, or levothyroxine. We calculated the prevalence of abnormal thyroid labs amongst hospitalized patients with AFib with RVR.
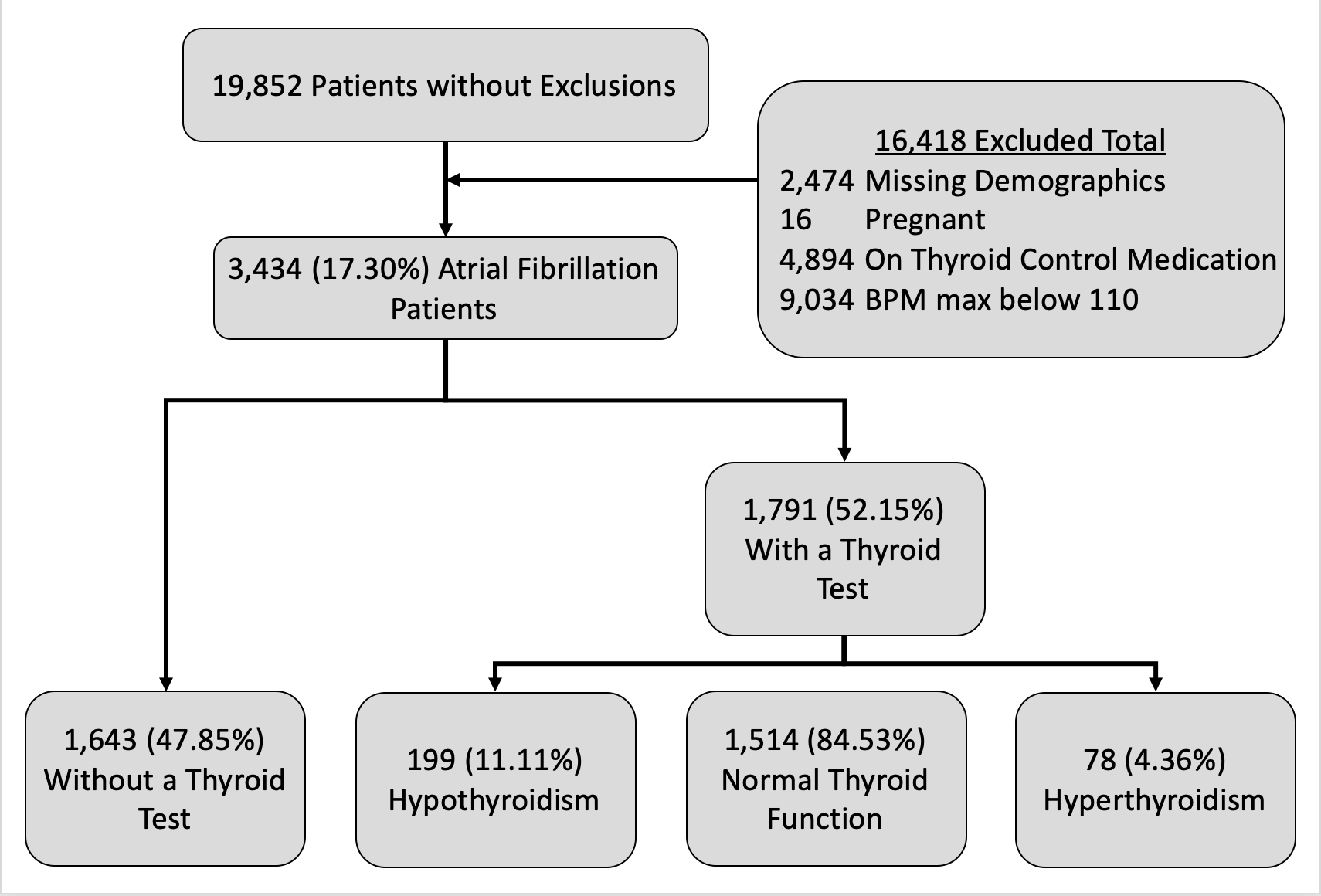
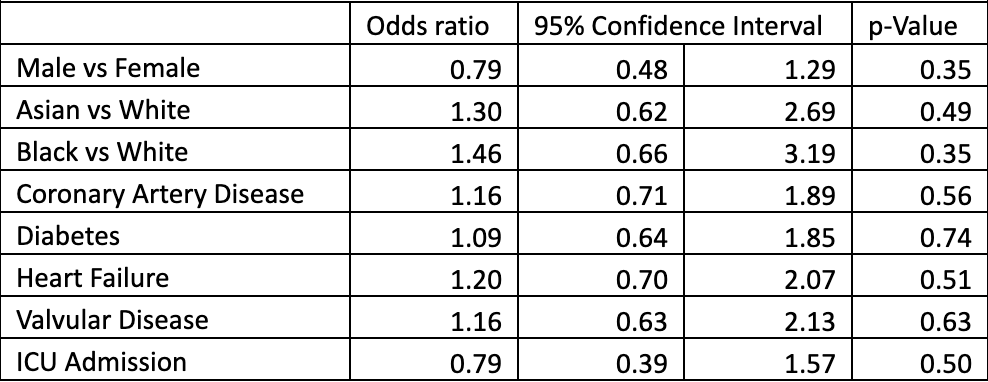
Results: 19,852 patients were identified to have had a diagnosis of atrial fibrillation. 16,418 patients were excluded mostly due to normal heart rate and existing thyroid medication. 1791 patients (52.15%) who passed exclusion criteria were tested for thyroid levels. Logistic regression analysis revealed ICU admission was associated with a higher odds of being tested (OR 1.55, p < 0.01) as was asian race (OR 1.37, p < 0.02). Of tested patients, 78 (4.36%) had a laboratory diagnosis of hyperthyroidism, 199 (11.11%) were found to have hypothyroidism, and 1514 patients (84.53%) had normal thyroid labs. 48.7% of hyperthyroid patients were women. Logistical regression analysis showed asian race and black race were associated with increased odds of hyperthyroidism vs normal test results (odds ratios 1.30 and 1.46). Patients with coronary artery disease (1.16), heart failure (1.20), and valvular disease (1.16) were found to have a higher odds ratio of hyperthyroidism. Being male and admitted to the ICU had lower odds ratio (0.79 and 0.79 respectively) for hyperthyroidism, though these results were not statistically significant.
Conclusions: Approximately half of patients hospitalized with AFib and RVR were tested for thyroid dysfunction, with ICU stay and asian race associated with increased testing. A small percentage of tested patients had abnormal thyroid labs suggestive of hyperthyroidism. Asian race, black race, female sex, CAD, heart failure, and valvular disease trended towards increased odds of testing positive for hyperthyroidism. Lack of statistical significance for hyperthyroid risk factors was likely due to the small number of hyperthyroid patients in our data but a larger data set may provide more power to detect these differences.