Background: Admitted patients with Type II Diabetes Mellitus (T2DM) are often placed on sliding scale insulin with four fingerstick blood glucose (FSBG) tests per day, regardless of home insulin use or baseline glycemic control. FSBG testing in the inpatient setting allows for real-time insulin adjustment to protect patients from significant hypo- or hyperglycemia, but FSBG monitoring of patients at low risk for inadequate glycemic control may add to nursing workload, cause patient discomfort, and waste resources without changing clinical care. This project was conceived prior to the COVID-19 pandemic, but was coincidentally operationalized after March 2020.
Purpose: Based on an initial needs assessment our student-led team identified an opportunity to reduce FSBG testing in patients with T2DM at low risk of poor glycemic control on the Hospital Medicine service at an urban, academic 1,100-bed tertiary care center.
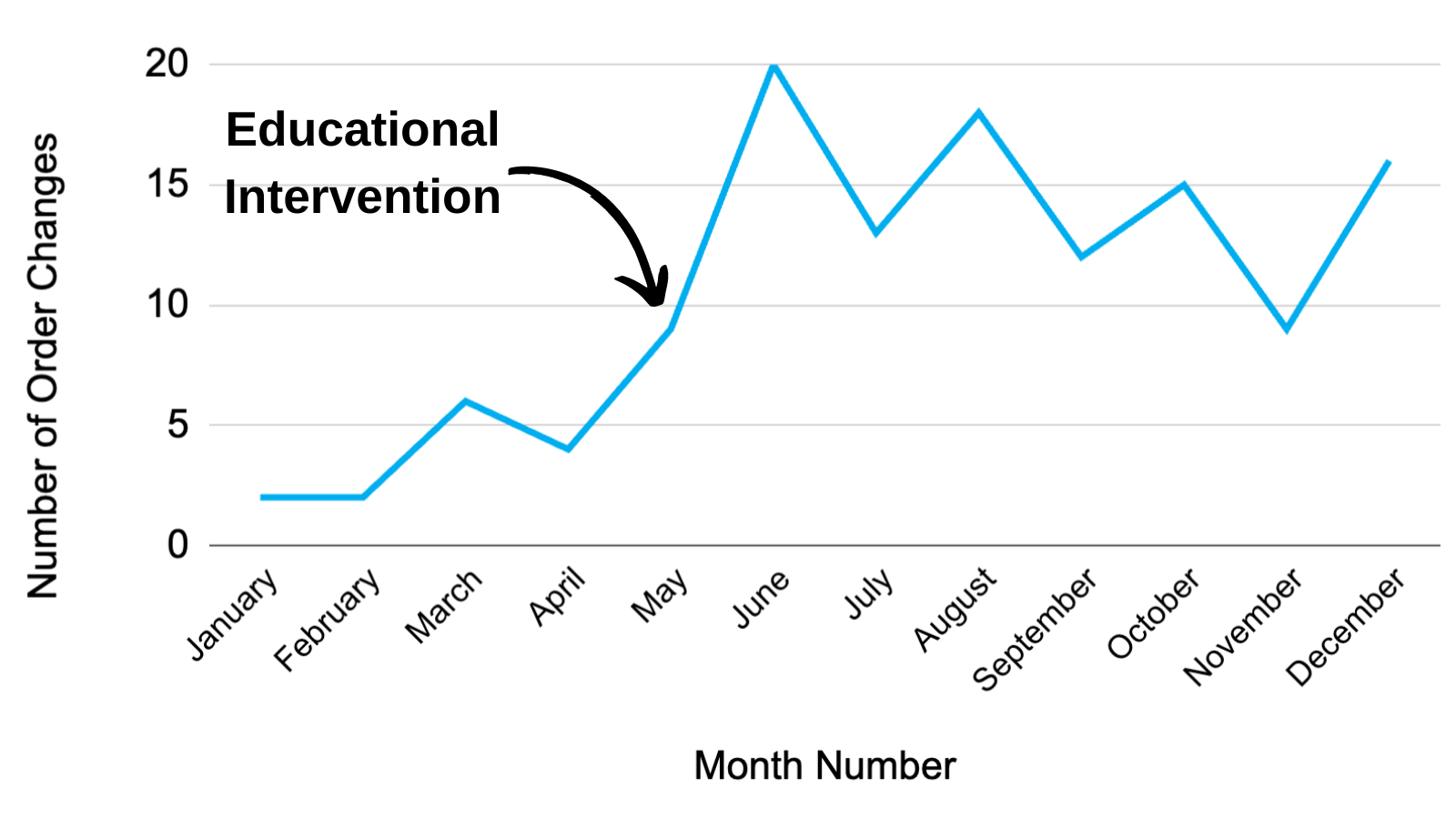
Description: The needs assessment was performed in October 2019 and included a point prevalence study (PPS) of FSBG testing in patients on the hospital medicine service, a provider awareness study (PAS) of FSBG testing, and a nurse perception survey (NPS). These showed that FSBG testing is common, provider awareness of FSBG monitoring is low, and nurses estimate that they require 4-10 minutes per FSBG when preparation and clean-up time was included. Providers were likely to underestimate the number of patients receiving FSBG testing.1 These findings informed a multifaceted student-led intervention that included an electronic and educational component. Pre-intervention data (January 1 to May 31 2020) was compared to post-intervention (June 1 to December 31 2020). The project was a collaboration between Hospital Medicine and Endocrinology. The first component included adding a twice daily before meals (BID AC) order option for FSBG monitoring in the electronic medical record (EMR). The second component involved educational outreach to inform clinical stakeholders that certain patients with T2DM qualified as “low-risk” for poor glycemic control and to explain the BID AC FSBG order change. Patients were considered “low-risk” if they were 1) not on home insulin, 2) had a 72-hour average FSBG less than 250 mg/dl, 3) received total daily dose of insulin less than five units, 4) were not on medications that cause hyperglycemia such as steroids. The program was named “Click It Before You Stick It”, referring to the need to adjust the EMR order prior to FSBG testing.Outcome measures included the number of FSBG order changes per month, the proportion of patients with T2DM receiving BID FSBG or no FSBG testing daily, and the total number of FSBG tests avoided per month. The EMR FSBG order change occurred prior to the educational intervention, so there was a small change in FSBG orders during the pre-intervention period. After the educational intervention, there was a 208% relative increase in order changes per month from 4.60 to 14.71 (p< 0.01). The proportion of qualifying patients whose FSBG order changed from 2.9% to 4.9%, and 1,541 FSBG tests were avoided, yielding an estimated cost savings of $13,868.
Conclusions: This student-led intervention targeting overuse of FSBG testing in patients at low risk for poor glycemic control led to a statistically significant reduction in FSBG testing. The overall uptake and financial impact were lower than expected. FSBG remains a potential target for improved value in inpatient medicine.