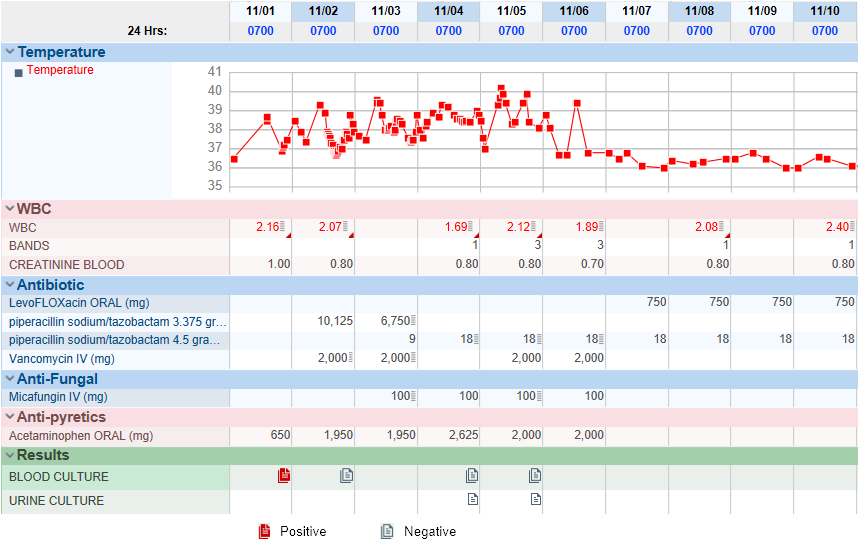
Case Presentation: A 69-year-old male with history of iron deficiency anemia, recurrent venous thromboembolism on apixaban, splenomegaly, ulcerative colitis who presented to emergency department due to exertional shortness of breath. 6 weeks prior to admission, the dose of azathioprine was increased from 50mg daily to 100mg daily due to suboptimal 6-thioguanine nucleotide (6-TGN) level. 1 week prior, he developed exertional shortness of breath and chest pain. CT pulmonary angiogram was unremarkable. CBC was significant for pancytopenia with WBC 2.43×10^9/L, hemoglobin 7.1 g/dL, platelet 80 ×10^9/L, which had decreased significantly in 6 weeks. Absolute neutrophil count was 1800 cells/µL. During his stay in the hospital, he was persistently hypotensive and anemic requiring 4 units of packed red blood cell and intravenous fluids. He developed spiking fever with temperature 39.6°C at maximum despite the use of vancomycin and piperacillin-tazobactam. Azathioprine was held on admission and 6-TGN level on day 5 was 256 pmol/8×10^8. Given persistent FUO, micafungin was started. Venous duplex ultrasound was positive for right acute deep tibial venous thrombosis. Therapeutic anticoagulants were unable to be initiated due to severe thrombocytopenia. On day 4, blood culture obtained on admission turned positive for gram negative rods. The pathogen was finally identified as R. mucosa on day 5. Even though blood cultures had cleared since admission, the patient was persistently febrile. Further studies including PET/CT scan, CT of abdomen and pelvis, transthoracic echocardiogram, were all unremarkable. Susceptibility test was unable to proceed in absence of Clinical & Laboratory Standards Institute guidelines, thus a trial of intravenous levofloxacin was started which resolved his fever completely. Patient was discharged on intravenous piperacillin-tazobactam and oral levofloxacin to complete a 2-week course of antibiotics.
Discussion: Roseomonas mucosa is a slow-growing gram-negative, aerobic, pink-pigmented, coccobacilli. It is an opportunistic pathogen with most infections reported in immunocompromised patients, including patients with chronic steroid use, AIDS, acute lymphoblastic leukemia, organ transplantation, leading into bacteremia, peritonitis, infective endocarditis. In our case, the patient was immunocompromised due to pancytopenia secondary to azathioprine. The t1/2 of 6-TGN is about 5 days. His 6-TGN level of 256 pmol/8×10^8 on day 5 indicates a myelotoxic level of greater than 500 pmol/8×10^8 prior to the admission. Extensive workups for fever of unknown origin (FUO) were only remarkable for venous thromboembolism, which was initially thought to be the cause, as bacteremia had cleared with piperacillin-tazobactam. However, in general, R. mucosa was consistently resistant to cefepime, ceftazidime, ampicillin and frequently resistant to trimethoprim-sulfamethoxazole, ceftriaxone, piperacillin-tazobactam, with consistent susceptibility to amikacin and ciprofloxacin. Given a complete resolution of fever following levofloxacin, R. mucosa is believed to cause the FUO. This case illustrates R. mucosa bacteremia as a possible cause of FUO and appropriate selection of antibiotics is important.
Conclusions: Azathioprine induced pancytopenia can lead to Roseomonas mucosa bacteremia, which may present as fever of unknown origin. R. mucosa is resistant to multiple antibiotics, therefore appropriate use of antibiotics is important.