Case Presentation: A 45 year old woman with a past medical history of ESRD on hemodialysis, antiphospholipid syndrome on warfarin, and type 2 diabetes presented with severe, diffuse, intermittent abdominal pain. Physical exam was notable for tender subcutaneous nodules in the lower abdomen associated with overlying violaceous patches and central necrosis. Labs were notable for creatinine: 8.02 mg/dL, calcium: 10.3 mg/dL, phosphorus: 6.7 mg/dL, PTH: 231 pg/mL, INR: 2.3, normal liver function tests, and no leukocytosis. Skin biopsy demonstrated necrotic tissue with vasculopathic reaction in the dermis, but no definitive evidence of intravascular calcification. After interdisciplinary discussions with dermatology, nephrology, and hematology, the diagnosis of calciphylaxis was made. The patient was initiated on treatment with sodium thiosulfate during her hemodialysis sessions, with slow improvement of her abdominal pain. Her phosphate binder was transitioned from calcium acetate to sevelamer carbonate. Additionally, given the risks of worsening calciphylaxis with warfarin, she was switched to apixaban despite the risk for being subtherapeutic due to her antiphospholipid syndrome.
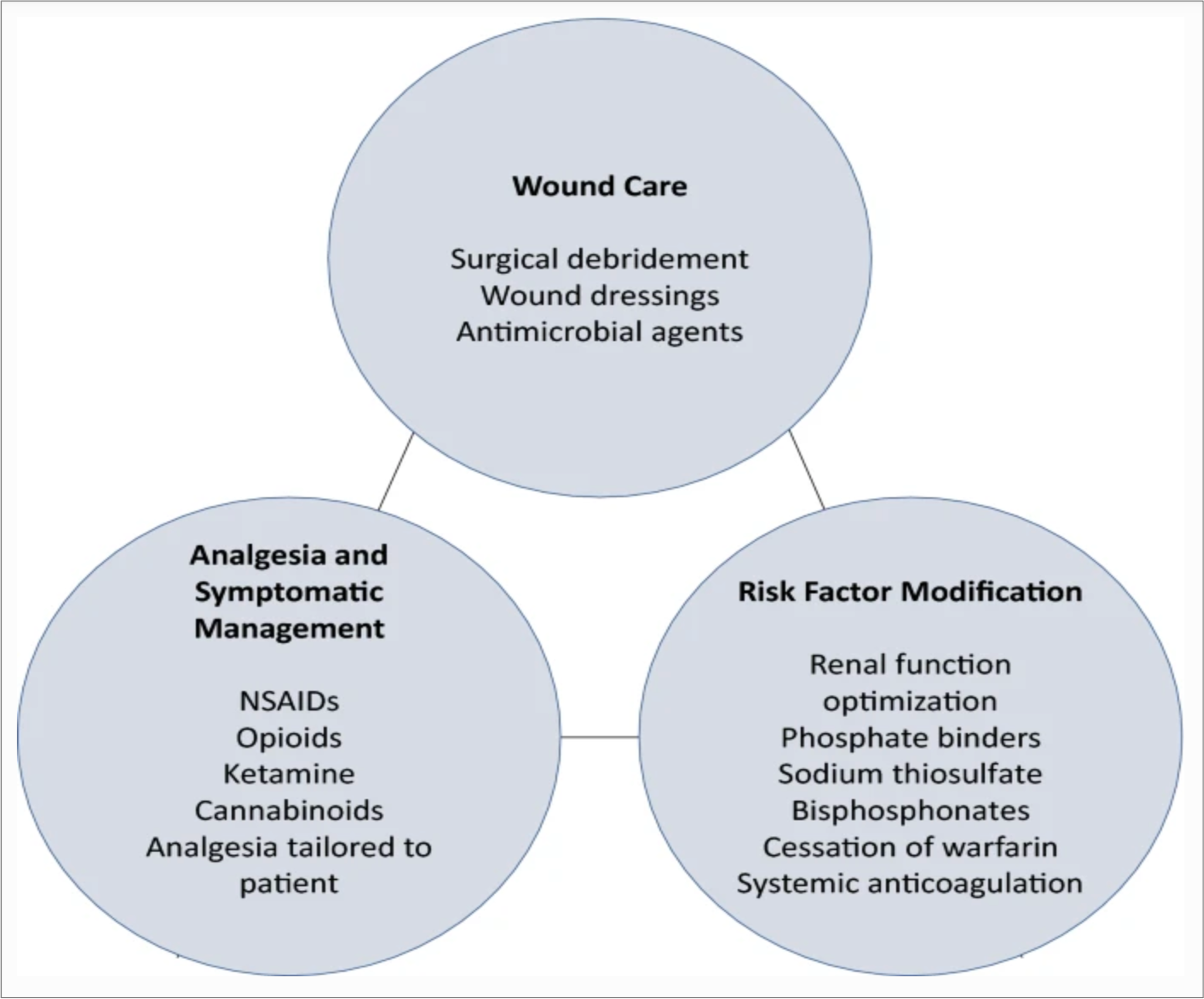
Discussion: Calciphylaxis or calcemic uremic arteriolopathy, is a painful, often under-recognized disease that predominantly occurs in End-Stage Renal Disease (ESRD) patients. Calciphylaxis is a highly morbid disease with one-year mortality rates ranging from 45-80%. Early recognition and involvement of a multidisciplinary team is critical for management. The differential diagnosis for our patient included calciphylaxis, panniculitis, warfarin-associated skin necrosis, and cellulitis. Our patient had multiple risk factors for the development of calciphylaxis, including ESRD on calcium supplementation, antiphospholipid syndrome on warfarin, and morbid obesity. The location of her lesions, in the subcutaneous adipose tissue of the abdomen, is also common in calciphylaxis. Interestingly, her biopsy did not definitively show calciphylaxis. With her multiple risk factors for calciphylaxis, the utility of a biopsy could be debated, especially given the risk of introducing infection. The management of her disease included multiple specialties; dermatology for consideration of biopsy; nephrology for optimization of her calcium and phosphate and initiation of sodium thiosulfate; hematology for management of her anticoagulation; and consistent wound care for her lesions. Unfortunately, the prognosis for patients with calciphylaxis remains poor despite appropriate management.
Conclusions: 1. Know that the diagnosis of calciphylaxis requires a high degree of clinical suspicion and recognition of the risk factors for the development of the disease.2. Recognise that the management of calciphylaxis requires a multidisciplinary approach.