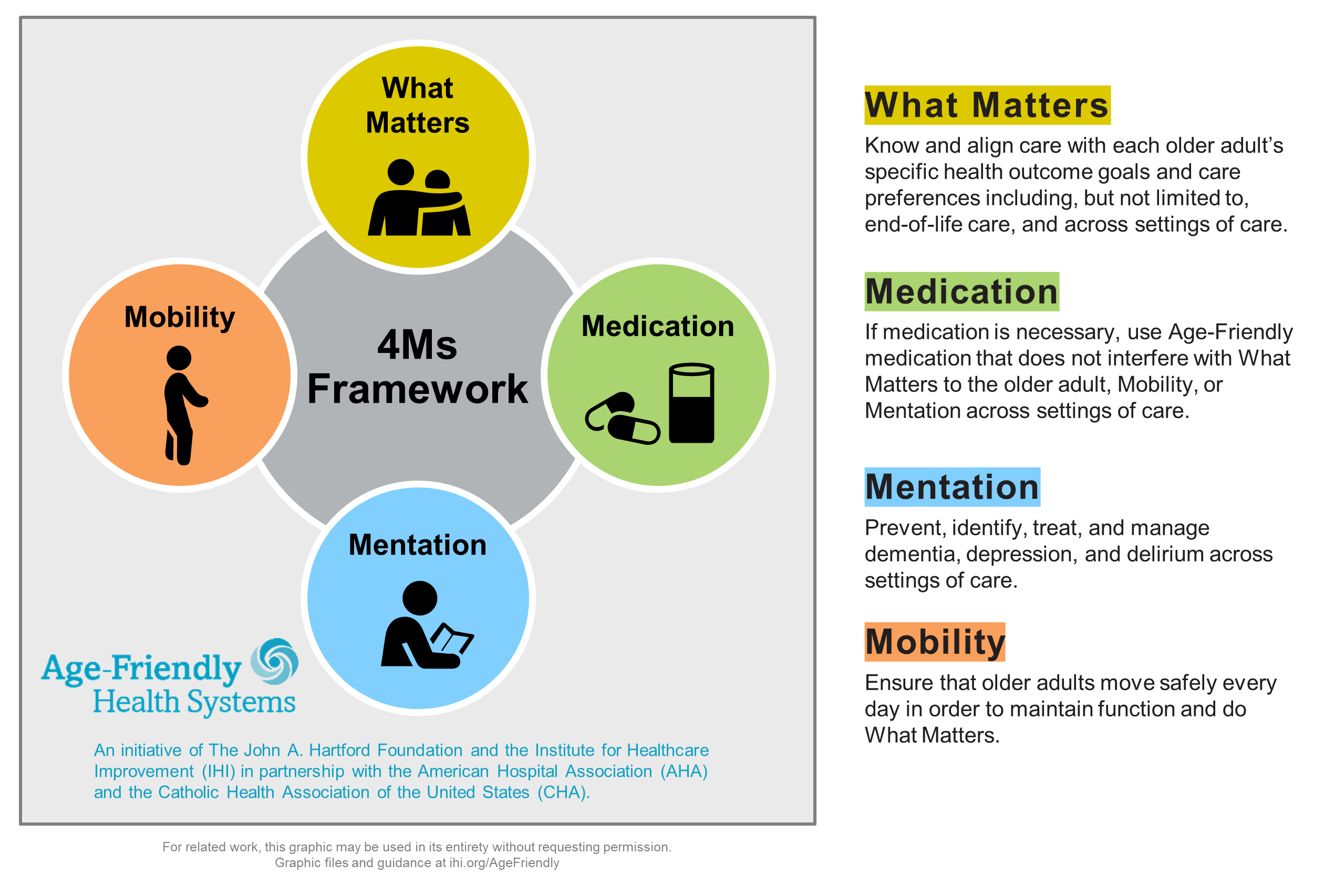
Case Presentation: Planning a safe discharge from the hospital is a collaboration that includes the care team and the patient. At our VA hospital, a geriatric 4M’s (Mobility, Medications, Mentation, What Matters Most) assessment helps to determine “What Matters Most” to older Veterans as well as to connect them with the right community services (such as meals, transportation, caregiver support) and medical referrals (such as audiology, optometry, podiatry, cognitive assessment) at the right time. This framework helps to frame care in a patient-centered way, especially in the setting of complex or prolonged hospitalizations. Mr. M, a 75 year old male Veteran, with a past medical history including congestive heart failure (ejection fraction 25-35%) was admitted to the hospital for shortness of breath and lower extremity edema with associated wounds. Initial treatment included titration of cardiac medications and ongoing diuresis. In the first few days of hospitalization, the care team expressed concerns about his cognition and of the Veteran’s ability to care for himself at home. The team consulted both physical and occupational therapy (PT and OT) to assess his functional status, including activities of daily living (ADLs) and instrumental activities of daily living (iADLs). Initial recommendations were for short stay rehab (SSR). A 4M’s assessment was completed with the Veteran on hospital day 2 to determine “What Matters < ost,” which was being at home and his independence. He stated during this time he would not want SSR at time of discharge.Given the severity of his heart failure, the patient required hospitalization over a period of 6 weeks for ongoing diuresis, including transfer to the medical intensive care unit (MSICU) for cardiogenic shock. The cardiology team recommended a mitral clip to improve his cardiac function which was completed on week 2. During the weeks of hospitalization Mr. M received care from 5 MSICU attendings, 5 medicine attendings, 8 resident physicians, 5 case managers, 3 PTs, 3 OTs and one social worker. PT was reconsulted four times to help determine placement, with continued recommendations for SSR.In line with the Veteran’s stated goals for returning home, he worked with PT/OT and nursing staff during the hospitalization, and was able to regain much of his strength, ambulating 250 feet and becoming modified independent in ADLs. His cognition and mental status also improved as he recovered from his acute illness. A detailed assessment of his functional status and home environment also identified additional needs, including home health services and outpatient referrals for wound care, audiology, optometry, pain clinic, and transportation assistance. The team was able to identify a close friend who could provide some help, and the patient was eventually discharged home with these supports and services in place.
Discussion: The geriatric 4M’s framework can provide a way for the patient’s voice to be heard in a setting where there is frequent and rapid turnover of care team members. In this case, the interdisciplinary team was able to align with the patient’s goals and identify supports and services that would allow him to maintain independence in his home.
Conclusions: Early 4M’s assessments in hospitalized older Veterans can help facilitate safe discharge planning that is consistent with “what Matters most” to them.