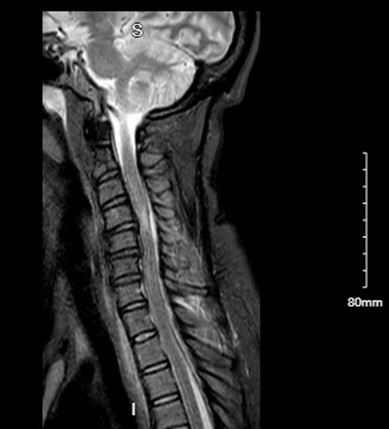
Case Presentation: A 42-year-old female presented with two days of fever, dysuria, and hematuria, associated with upper and lower back pain, body aches, and anorexia. She had no significant past medical history and no recent surgical procedures. She denied tobacco, alcohol, and intravenous drug use. The exam was significant for suprapubic pain and left costovertebral angle tenderness, as well as antalgic gait. Initial labs were notable for WBC of 20,000/mcL and pyuria (>50 WBCs per high power field), and incidental positive COVID-19 PCR. Intravenous ceftriaxone was started for a suspected urinary tract infection. The next day, the patient became lethargic and developed neck stiffness and rapidly progressive ascending paresis of bilateral lower extremities and distal upper extremities. MRI of cervical, thoracic, and lumbar spine revealed a large dorsal cervicothoracic epidural abscess extending from C4 to T3 with cord compression at C4. The patient underwent C3-T2 laminectomies and was treated with a six-week course of Ceftriaxone. Surgical cultures grew beta-hemolytic Group A Streptococcus while blood cultures grew no organisms. One week post-operation, the patient was still paraplegic. After three months of intensive physical therapy, the patient improved clinically, was able to flex her foot and knee, and slowly lift up her left arm but continues to be dependent for activities of daily living.
Discussion: Spinal epidural abscess (SEA) is a suppurative collection between the dura and the vertebral column. Pathogenic bacteria gain entry to the epidural space from the infected contiguous structures or hematogenous seeding from skin or soft tissue infections. Diagnosis of SEA is often delayed due to its myriad presentations – back pain (85%), paraplegia (39%) fever (32%), paraparesis (32%) deep tendon reflex changes (21%), paresthesias (39%), bowel or bladder incontinence (27%), no motor deficits (29%) and encephalopathy (11%), with a duration of 6 hours to 12 months (3,4,5). SEA should be considered for any patient with fever and back pain, even in the absence of neurological deficits. Prompt workup and intervention are vital as delays in intervention correlate with adverse outcomes. The predominant etiological agent of SEA is Staphylococcus aureus (40-60%), gram-negative bacteria (15%), coagulase-negative Staphylococci 3%, and viridans group streptococci (9%). A unique feature of this case was the growth of Group A Streptococcus (GAS) from surgical cultures. Although SEA with Group A strep has been reported in children (in the setting of Varicella infection), this is the first reported case of GAS SEA in the adult population. Our patient had none of the usual risk factors for SEA. However, she tested positive for COVID-19. Case series of 6 primary SEA associated with COVID infection suggest this as another risk factor for SEA(7). Experts postulate immunocompromised state, nosocomial superinfection, or endothelial damage induced by COVID as a possible mechanism that favors retrograde invasion of the spinal cord (7).
Conclusions: Spinal epidural abscess (SEA) is a rare, potentially fatal illness with increasing prevalence. Despite advances in neuroimaging and treatment, SEA remains a formidable disease due to frequent delays in diagnosis, rapid progression to irreversible neurological deficits, and uncontrolled sepsis.Although SEA is a rare condition, awareness of its diagnostic pitfalls can aid in timely diagnosis and treatment which portends a favorable outcome.