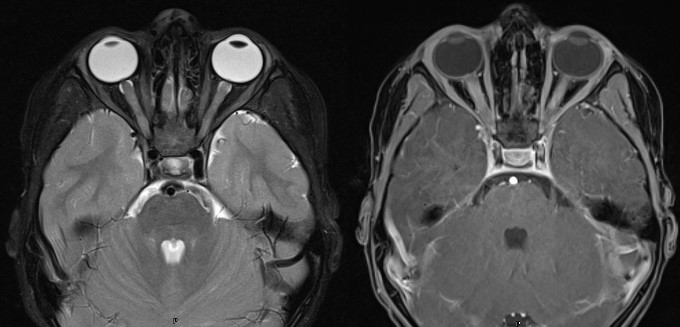
Case Presentation: A 5-year-old male presented to an outside hospital with one month of headaches, decreased visual acuity (VA) and color vision, and one day of vomiting. Workup included CT brain and venogram with an incidental corpus callosum cyst, ESR of 19 (0-15 mm/hr), and normal blood counts, CRP, and metabolic and hepatic panels. Ophthalmologic exam revealed bilateral 3+ optic disc edema and VA deficit, 20/800 on the right and 20/100 on the left. He received one dose of intravenous (IV) Solumedrol and Acetazolamide 14 hours prior to transfer. On arrival, LP had a normal opening pressure (OP), protein, glucose and cell count, and MRI brain/orbits showed bilateral optic nerve edema, consistent with optic neuritis (ON). Serum Lyme IgG was positive, and IgM was equivocal, without typical symptoms of Lyme. Toxoplasma IgG and CSF oligoclonal bands returned positive without other signs of toxoplasmosis or multiple sclerosis (MS). Arbovirus, West Nile Virus, HSV, infectious encephalitis panel, ANA, ACE, B12, Lysozyme, MMA, bartonella, NMO/AQP4 and MOG-IGG1 were unremarkable. He was treated with five days of IV Solumedrol (15 mg/kg twice a day). He was discharged with a 4-week prednisone taper, with resolution of headache and improvement of VA (20/60 bilaterally) two days after discharge. Later, when Lyme Western Blot resulted with 5 IgG and 2 IgM bands in the serum and 4 IgG bands in the CSF, patient was initiated on Doxycycline (4.4 mg/kg/day) for 2 weeks per IDSA guidelines. Four weeks later, his VA was 20/30 bilaterally with a normal Isahara test.
Discussion: Pediatric ON is a clinical diagnosis with an incidence of 0.9-1.66 per 100,000 person years and may be caused by genetic or demyelinating diseases, infection, or neoplasm. ON typically presents with deficits of VA, color vision and visual fields, as well as pain with eye movements, often described as a headache. Lyme ON is extremely rare, especially in the pediatric population, and is diagnosed with serum and CSF Lyme studies in conjunction with MRI brain/orbits. Ceftriaxone, doxycycline, penicillin G, and cefotaxime are effective treatments. The five documented cases of pediatric Lyme ON were treated with doxycycline and/or IV Ceftriaxone, with or without IV Solumedrol. Of the four cases with reported clinical outcomes, three cases had clinical resolution of symptoms at four months, and one case resulted in permanent blindness. To our knowledge, this is the first reported pediatric case of ON due to Lyme with no other classic symptoms, such as erythema migrans, arthralgias, and myalgias. Of note, it is unlikely that a single dose of Acetazolamide 14 hours prior to LP affected the OP.
Conclusions: Our case emphasizes the importance of considering Lyme in all cases of ON in Lyme endemic areas, as early diagnosis and treatment can prevent permanent vision loss.