Background: Email represents an administrative burden which contributes to overall burnout. While general strategies to mitigate burnout related to email have been published (Armstrong 2017), formal clinical workplace guidelines and specifically their impact have not been described in the literature. The University of Michigan (UM) Division of Hospital Medicine (HM) developed and distributed email management guidelines to faculty and staff in February 2023. These guidelines created expected norms for faculty and staff to not manage emails during non-work time and created best practices to ensure that important emails do not get missed. The purpose of this study is to use the RE-AIM framework (https://re-aim.org/) to assess reach, effectiveness, adoption, and implementation of email guidelines in an academic HM division.
Methods: Email guidelines were implemented via email February 2023, followed by announcements at division-wide 3 monthly HM business meetings, 1 case conference, 2 email reminders, and posting to HM website and flyers in work rooms. UM HM emailed an online, anonymous survey October – November 2023 to all faculty and staff: 145 faculty, 45 advanced practice providers, 8 clinical and resident assistants, and 39 administrative staff members (n=237). We assessed demographics (job role, gender, race/ethnicity, caregiving status, years’ experience) and email management (reach = awareness of guidelines; effectiveness = email contribution to burnout, disconnecting from work emails during free time; adoption = personal use of guidelines, seeing guidelines in practice). We used univariate statistics (counts/percentage, mean/standard deviation) to determine prevalence for all measures and stratified email management responses by job role. We used bivariate and multivariate logistic regression to assess email guideline use associations with job role, gender, race/ethnicity, caregiver status, and years of experience.
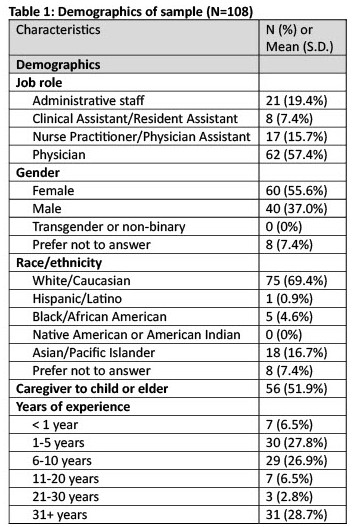
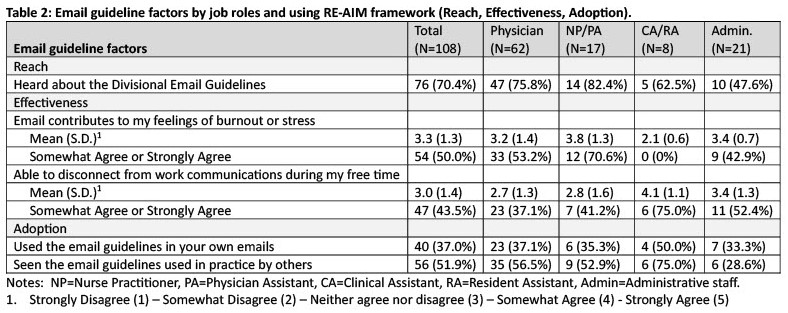
Results: Our response rate was 46% (108/237). Among 108 respondents, we had 62 (57%) physicians, 17 (16%) NP/PA’s, 8 (7%) clinical/resident assistants, 21 (19%) administrative staff, 60 (56%) female, 75 (69%) white, 56 (52%) caregivers to child or elder, and 30 (28%) 1-5 years’ experience (see Table 1). 76 (70%) heard about email guidelines, 54 (50%) agreed email contributes to burnout, 47 (44%) agreed they can disconnect from work communications during free time, 40 (37%) used email guidelines, and 55 (51%) had seen email guidelines used in practice. Using email guidelines was highest among clinical/resident assistants (4/8=50%) followed by physicians (23/62=37%). See Table 2 for other email guideline factors by job roles. In bivariate and multivariate analyses, email guideline use was associated with increasing years of experience.
Conclusions: Among responding faculty and staff in one academic HM division, nearly 1 in 2 experienced email-related burnout. Our implementation framework achieved adoption through multiple distributions over 9 months, demonstrated reach with nearly 3 in 4 responding faculty and staff aware of email guidelines, and showed effectiveness with over 2 in 5 responding faculty and staff able to disconnect from email during free time. Future assessments should focus not only on improving effectiveness, but also maintenance of these email guidelines.