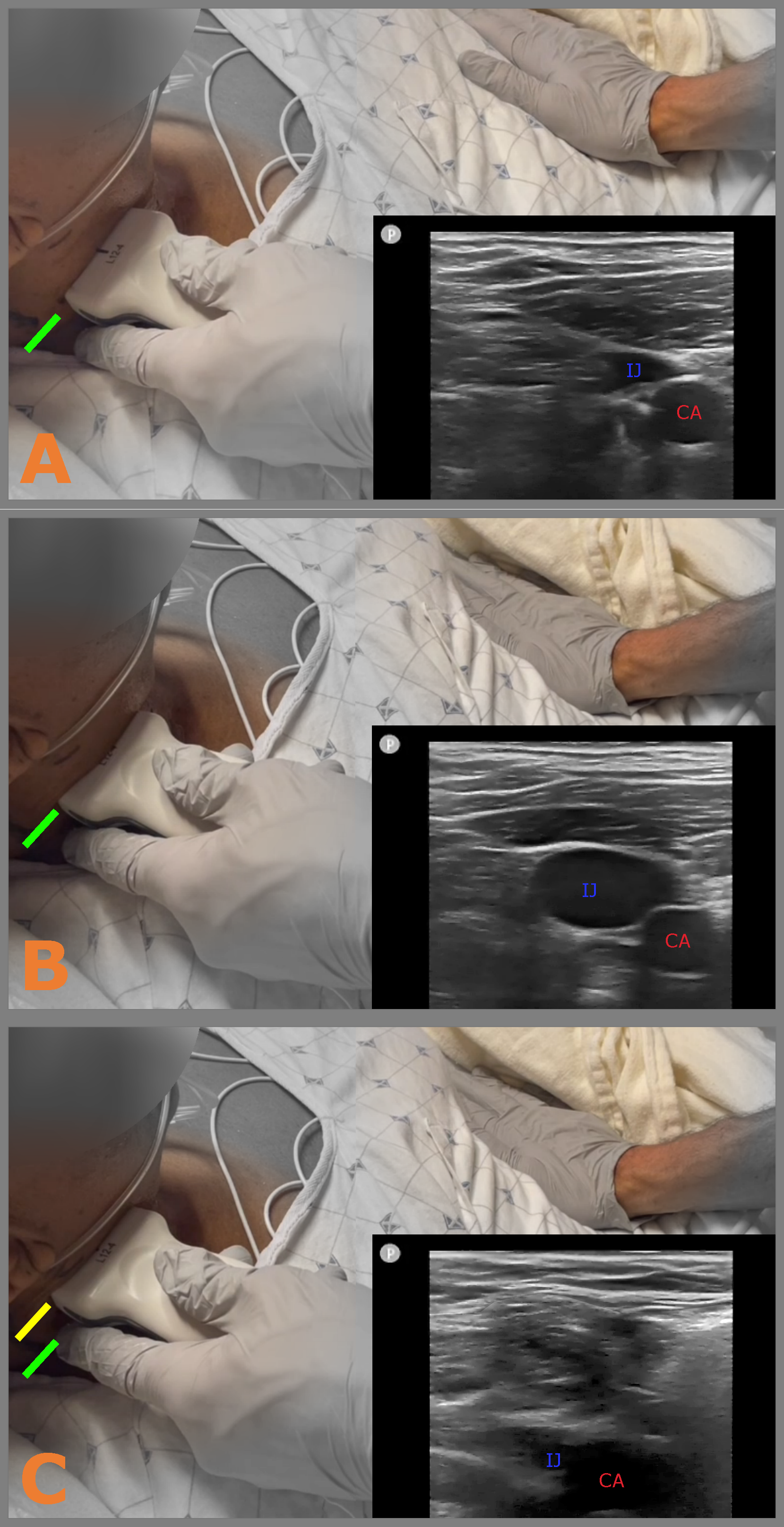
Background: The physical exam for heart failure can be limited by poor reproducibility, lack of specificity, provider inexperience, or patient habitus. To estimate the JVP or HJR requires identifying the internal jugular vein (IJV). Finding the IJV can be limited by those factors but the addition of ultrasound can improve its identification. Ultrasound can therefore be used to estimate jugular venous pressure (uJVP) and, as we describe here, the hepato-jugular reflux (uHJR).
Methods: Our objective was to determine the operating characteristics of uHJR and uJVP, and assess their correspondence to right atrial pressure (RAP) and pulmonary capillary wedge pressure (PCWP) measured via right heart catheterization (RHC). To accomplish this we recruited adults undergoing RHC at 3 U.S. academic hospitals.The uHJR and uJVP were measured by students before RHC with scanners blinded to all patient characteristics. Receiver-operating curve and associated operating characteristics were analyzed for the uHJR and uJVP compared to the RHC reference standards (RAP and PCWP).
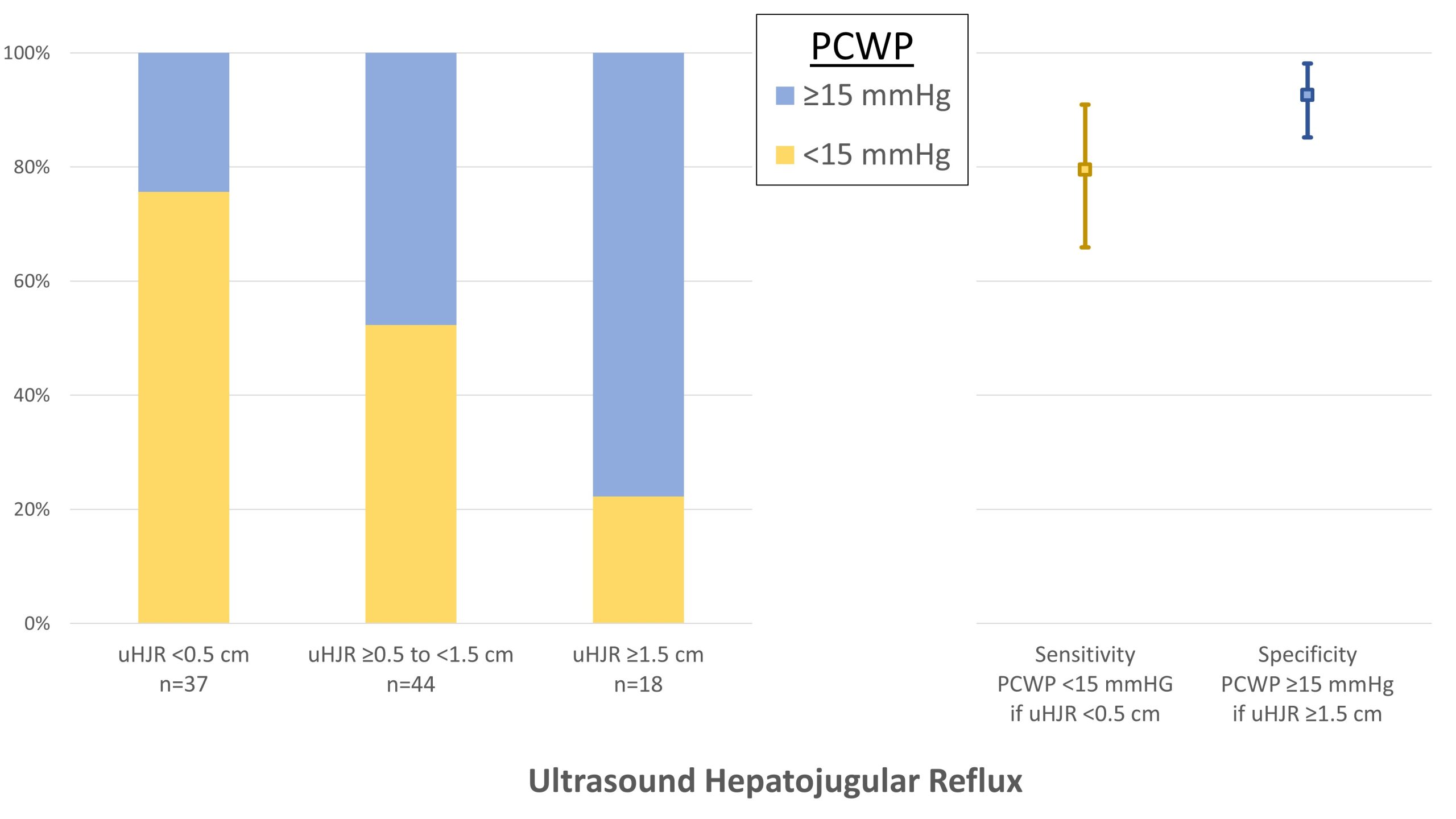
Results: A convenience sample of 107 patients was enrolled and eight were excluded for RHC cancellation or delay, with 99 remaining for analysis. Most were outpatients (55%) with the most common RHC indication being volume assessment (36.4%) or for a CAD or ACS work-up (34.3%). A total of 32 patients (32.3%) had a measured RAP ≥ 10 mmHg and 44 (44.4%) had a PCWP ≥ 15 mmHg. The uJVP was found to have an AUC of 0.68 (95% CI 0.57 – 0.79) for predicting a RAP ≥ 10 mmHg. The uHJR was found to have an AUC of 0.64 (95% CI 0.53 – 0.75) for predicting a RAP ≥ 10 mmHg. For predicting a PCWP ≥ 15 mmHg, the uJVP was found to have an AUC of 0.67 (95% CI 0.56 – 0.78) whereas the uHJR was found to have an AUC of 0.71 (95% CI 0.61 – 0.81).The uJVP and uHJR were measured in 0.5 cm increments, and the predictive ability varied at each increment. Rather than report a single threshold, we report multi-level thresholds that may be more useful to the practitioner. These thresholds were selected using the highest positive and negative LRs, respectively, that still allowed the majority of measurements to be classified as either PCWP < 15 mmHg or ≥ 15 mmHg. For excluding a PCWP ≥ 15 mmHg, a uJVP of ≤ 8 cm had a sensitivity of 82% (95% CI 70% to 94%) with a negative LR of 0.4. For predicting a PCWP ≥ 15 mmHg, a uJVP ≥ 11 cm had a specificity of 83% (95% CI 72% - 93%) and positive LR of 2.2.An uHJR that was unchanged (or zero cm increase) had a sensitivity of 80% (95% CI 66% to 91%) and a negative of LR 0.4 for excluding a PCWP ≥ 15 mmHg. Conversely, an uHJR ≥ 1.5cm had a specificity of 93% (95% CI 85% to 98%) and a positive LR of 4.3 for predicting PCWP ≥ 15 mmHg. These results are summarized in Figure 2.There were eleven scans that had duplicated measures of the uJVP and uHJR. The interobserver agreement on these scans for a uJVP ≥8.5 cm versus < 8.5 cm was minimal, kappa 0.29 (95% CI -0.26 - 0.85), while agreement for uHJR ≥1 cm versus < 1 cm was almost perfect, kappa 1 (95% CI 1 - 1).
Conclusions: In patients undergoing RHC, the uHJR is reproducible, not limited by habitus and requires little technical skill or ultrasound training. Based on our study, when the uHJR was unchanged it was a modest predictor of a normal PCWP, but when the uHJR was ≥ 1.5 cm, it was a relatively specific finding for elevated PCWP. In comparison, a uJVP ≥ 8.5cm was found to be a modest predictor of RAP ≥10mmHg and specific for a PCWP ≥ 15 mmHg when uJVP was ≥ 11.5cm. Though a minority, many participants had a uHJR or uJVP measured in a range unable to accurately predict PCWP.