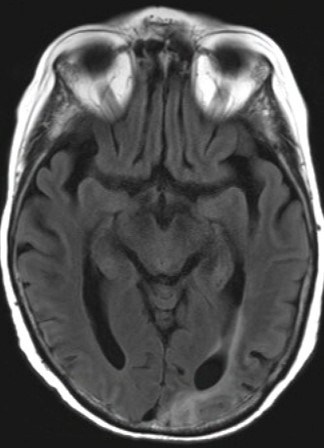
Case Presentation: A 62-year-old woman with Crohn’s disease and rheumatoid arthritis, on vedolizumab and prednisone, presented to the hospital with altered mental status. Her labs were notable for WBC 13.4K and creatinine 2.18mg/dL, CXR and non-contrast head CT were unremarkable. Blood cultures were obtained, and she was treated empirically with broad spectrum IV antibiotics and IV fluids. Despite resolution of her leukocytosis and AKI, her cognitive status declined, and blood cultures returned negative, so a broader evaluation was pursued, including viral, fungal, and rheumatologic studies, EEG, and LP. CMV PCR returned elevated at 3.4K IU/mL, CSF revealed WBC < 6 /L, protein 59 mg/dL, 82% lymphocytes, and negative infectious and auto-immune studies. Antibiotics were discontinued and she was started on valganciclovir 450mg daily. Her mental status worsened and she required a nasogastric tube for nutrition. Repeat brain MRI showed subcortical enhancement in the left frontal and occipital lobes. CSF fluid eventually returned positive for JC virus PCR, so she was started on a steroid taper. Her cognitive impairment remained, so a percutaneous endoscopic gastrostomy tube was placed, and she was discharged to a skilled nursing facility. Two weeks after discharge she was re-admitted to the hospital with septic shock and passed away soon after.
Discussion: Progressive multifocal leukoencephalopathy is a rare, fatal demyelinating disease of the CNS caused by JC polyomavirus reactivation and seen almost solely in immunocompromised individuals. Primary JC virus causes an asymptomatic infection, often in childhood that remains latent through cell-mediated immunity. Reactivation requires profound cellular immunosuppression, as seen in hematologic malignancies, organ transplantation, and immunomodulatory therapy. PML rose during the AIDS pandemic, declined following HAART, and remained rare until novel immunosuppressive therapies were introduced, notably natalizumab. Though initial symptoms vary depending on the location of CNS lesions, patients usually present with subacute neurologic deficits, such as AMS, weakness, or ataxia. Seizures, sensory loss, and headache are rare. There is no single criterion for diagnosis, but rather a combination of clinical, imaging, and virologic evidence is required. PML should be suspected in patients with consistent clinical features (subacute neurologic deficits with immunosuppression) and brain MRI with white matter lesions usually without mass effect. The diagnosis is certain when coupled with a positive CSF PCR for JCV.PML is a fatal disease for which no treatment exists. The median survival of patients without HIV or natalizumab use is three months. Survival is dependent on the ability to mount a cellular immune response to JCV, so the main approach is restoring the patient’s adaptive immune response by discontinuing immunosuppressive or immunomodulatory drugs and optimizing ART for patients with HIV.
Conclusions: AMS is a common presentation among hospitalized patients. The differential diagnosis is broad but the most common etiologies in the elderly include stroke or infections, an elusive diagnosis is seldom the cause. This case demonstrates a familiar presentation of AMS with a rare etiology and underscores the importance of maintaining clinical vigilance in the face of common presentations. While the familiarity of routine cases may lull us into complacency, it is crucial to remember that uncommon and rare diseases can masquerade as more typical conditions.