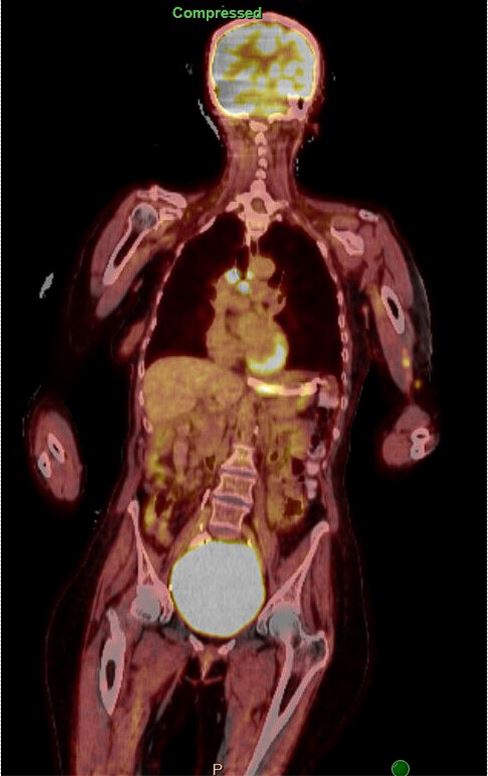
Case Presentation: A 65-year-old female with a history of focal epilepsy and carotid stenosis with recent endarterectomy presented with four weeks of abrupt aphasia, right sided weakness and several days of altered mental status and unusual left-hand movements. Since the endarterectomy one month prior to presentation, her family reported cognitive decline, memory loss and increased tremor activity. Her symptoms were initially attributed to cerebral hyper-perfusion syndrome with concern for inadequate seizure control, resulting in medication titration. The current admission had cEEG monitoring with multiple subclinical seizures and multifocal spikes over the left temporal, right temporal and left posterior head regions. CT scans demonstrated carinal and mediastinal lymphadenopathy, and no significant findings in the abdomen or pelvis. Serum autoimmune encephalopathy panel was positive for AB P/Q calcium channel binding antibody and Anti-Hu Positivity. LP findings were normal, except for Anti-Hu positivity. MRI showed resolution of the edema involving the left hippocampus and subtle flair hyperintensity in the left pulvinar. With continued seizure activity, epileptology and neuroimmunology decided on empiric steroid therapy with 1 gram of methylprednisolone for a 5-day interval with adjuvant apheresis (PLEX) resulting in stability of her seizure medications. A PET scan on HD14 demonstrated hypermetabolic brain lesions in the left temporal lobe lesion, left lateral occipital lobe lesion, multiple intensely avid mediastinal LNs, and subcarinal lymph nodes. Bronchoscopy with EBUS and biopsy was completed. Pathology revealed Small Cell Neuroendocrine Carcinoma with positive AE1/AE3, synaptophysin, chromogranin, and negative CD45. The final diagnosis was paraneoplastic limbic encephalitis. The patient was then transferred to the oncology team to start carboplatin and etoposide.
Discussion: Small Cell lung carcinoma is considered a primary lung cancer with a neuroendocrine origin. Patients with SCLC may have an associated paraneoplastic syndrome at a rate of approximately 9%. Although paraneoplastic limbic encephalitis is a rare condition with an annual incidence of 1 in 1.5-to-9-million-person years, it occurs in about 1 in 300 patients with cancer. Typical presentations include a subacute onset of working memory deficits, psychiatric changes, or seizures with a higher suspicion in those who may have underlying malignancy. Diagnosis is then confirmed with imaging, serum/CSF analysis, and EEG patterns. The PNS-Care diagnosis score can also assist in diagnosis. Treatment is management of the underlying malignancy, although steroids and IVIG are recommended to improve the neurologic symptoms. In our case, we demonstrate that PLEX can be an effective and well tolerated therapy.
Conclusions: Paraneoplastic syndromes should be maintained in the differential diagnosis for patients with subacute neurological changes or refractory seizures. The aim of this case report is to add to the case series available on paraneoplastic limbic encephalitis, as well as provide evidence for the role of PLEX therapy in its management along with the previously reported corticosteroids and IVIG. Rates of full recovery with treatment are low (< 10%), but treatment of the underlying cancer can lead to stabilization and improvement of symptoms.