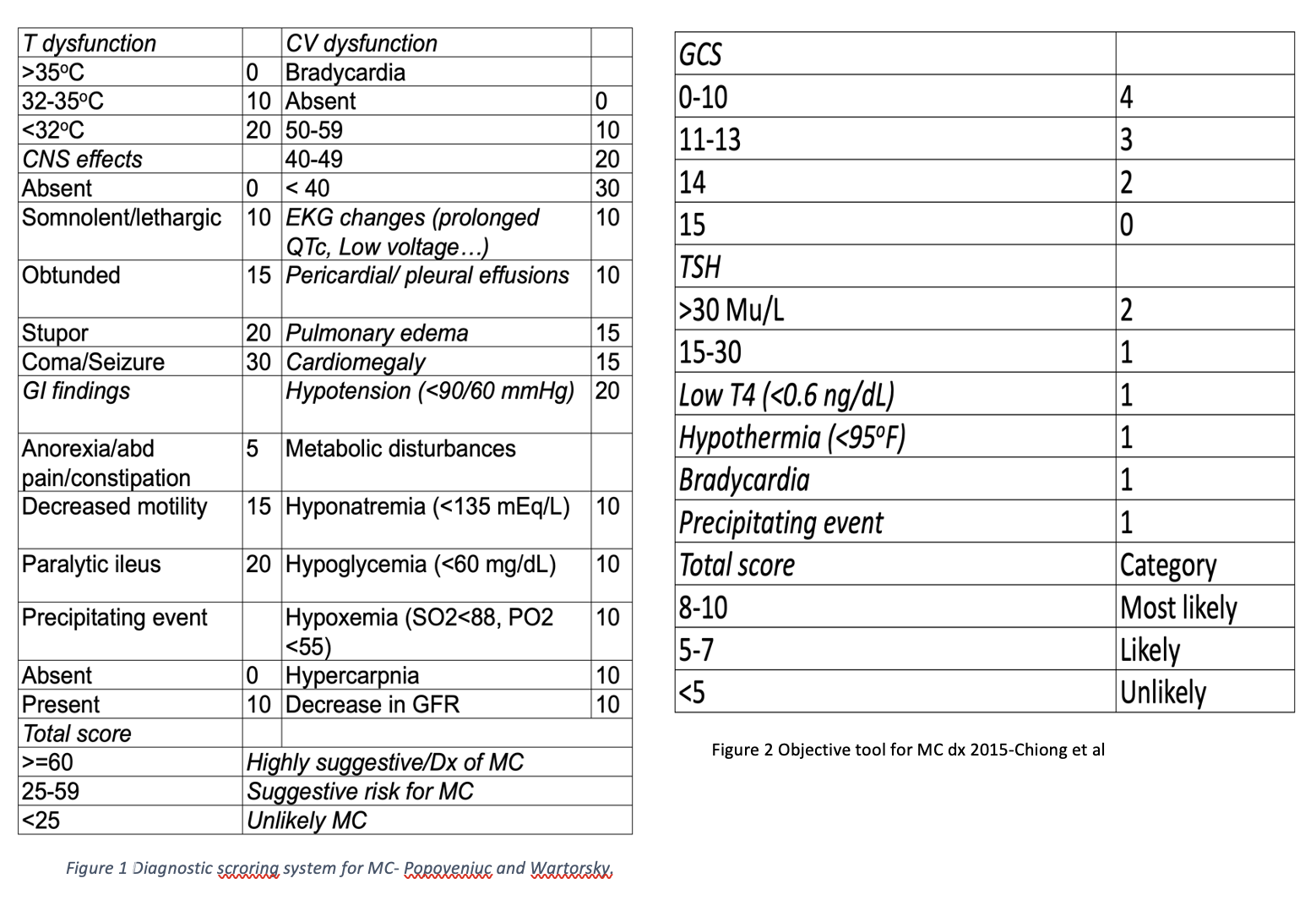
Case Presentation: A 45-year-old female with past medical history of gastric sleeve in 2018 and follicular thyroid carcinoma status-post total thyroidectomy in 2019, resulting in hypothyroidism, is currently taking Levothyroxine 200mcg daily. Patient presented to the Emergency department with increasing fatigue for the past 3 weeks. She reported progressive shortness of breath on exertion, “loss of energy”, cold intolerance, lower extremity edema bilaterally and constipation. She denied any chest pain, palpitation, or headache. On physical examination, vital signs: temperature 96.8oF, heart rate 54 bpm, blood pressure 97/70 mmHg, SpO2 98% on room air, respiratory rate 18 per minute. She appeared fatigued, lethargic but arousable during the conversation, and was alert, oriented to self, place, and time. An old surgical scar was noted on anterior neck. Non-pitting edema was noted in lower extremities bilaterally. The rest of the examination was unremarkable. Laboratory findings showed significant hypoglycemia with level of 42 mg/dl and HbA1C 4.7%. Patient was given juice and intravenous dextrose 50%. Further evaluation revealed thyroid stimulating hormone (TSH) 129.7mIU/l[normal range: 0.27-4.2mIU/l], FT4 0.2 ng/dl [0.76- 1.46 ng/dl], FT3 < 0.5 pg/ml [2.18-3.98pg/ml], morning serum cortisol 17.3mcg/dl [>10mcg/dl], ACTH < 5pg/ml [6-50 pg/ml]. An electrocardiogram showed sinus rhythm with low voltage on precordial leads. Given the patient's history of hypothyroidism, clinical presentation and lab findings, myxedema coma complicated by class 2 hypoglycemia was suspected. Using the 2 common myxedema coma scoring systems5,6, our patient scored 55 and 7, suggesting of myxedema coma which was a thyroid emergency. She was given levothyroxine 500mcg loading dose and hydrocortisone 100 mg every 8 hours intravenously and was admitted to the progressive care unit for close monitoring. Comprehensive history taking revealed patient recently consumed cranberry juice and grapefruit juice in the morning before taking Levothyroxine, which could interfere with levothyroxine absorption. Three days later, the patient improved mentally and physically.
Discussion: Myxedema coma is one of two thyroid emergencies in clinical practice3 with the incidence of 0.22 cases/mil/year7 but the mortality is high (25%-60%)4. Treatment includes high dose intravenous levothyroxine which may carry a risk of arrhythmia; therefore, closely monitoring patients during hospitalization is essential. Exploring precipitating factors is necessary to prevent the patient from an emergency event. In our case, there are multifactorial such as absorption interference, winter season2, and malabsorption (history of gastric sleeve). Also, hypoglycemia in a non-diabetic patient is unusual in daily practice1 and underlying causes need to be further investigated. In our case, myxedema coma is the underlying etiology.
Conclusions: -Hypoglycemia in a non-diabetic patient is an uncommon presentation1, especially in the setting of thyroid emergency scenarios such as myxedema coma. Given the rare incidence of 0.22 cases/mil/year2 but high mortality of 25-60%3,4, recognition of severe hypothyroidism/myxedema coma, precipitating factors, and prompt treatment are essential.-It is important to always reinforce correct levothyroxine taking to avoid severe hypothyroidism or myxedema coma.