Background: Asthma disproportionately affects racial minorities and individuals of lower socioeconomic status (SES). The introduction of biologic therapies in 2015 provided new treatment options for managing severe asthma. This study investigates the impact of biologics on racial and SES disparities in asthma-related emergency care visits before and after 2015.
Methods: Data from the National Health and Nutrition Examination Survey (NHANES) were analyzed for two time periods: pre-biologics (2009–2014) and post-biologics (2015–2020). Participants aged 18–64 who self-reported an asthma diagnosis were included in the study. The primary outcome was emergency care visits for asthma within the past year. Key independent variables were race/ethnicity (Non-Hispanic Black, Non-Hispanic White, Mexican American, Other races including Multi-Racial) and SES, measured by the ratio of family income to poverty. Descriptive statistics were calculated, and logistic regression models were used to assess associations between race, SES, and emergency care visits for asthma in each period.
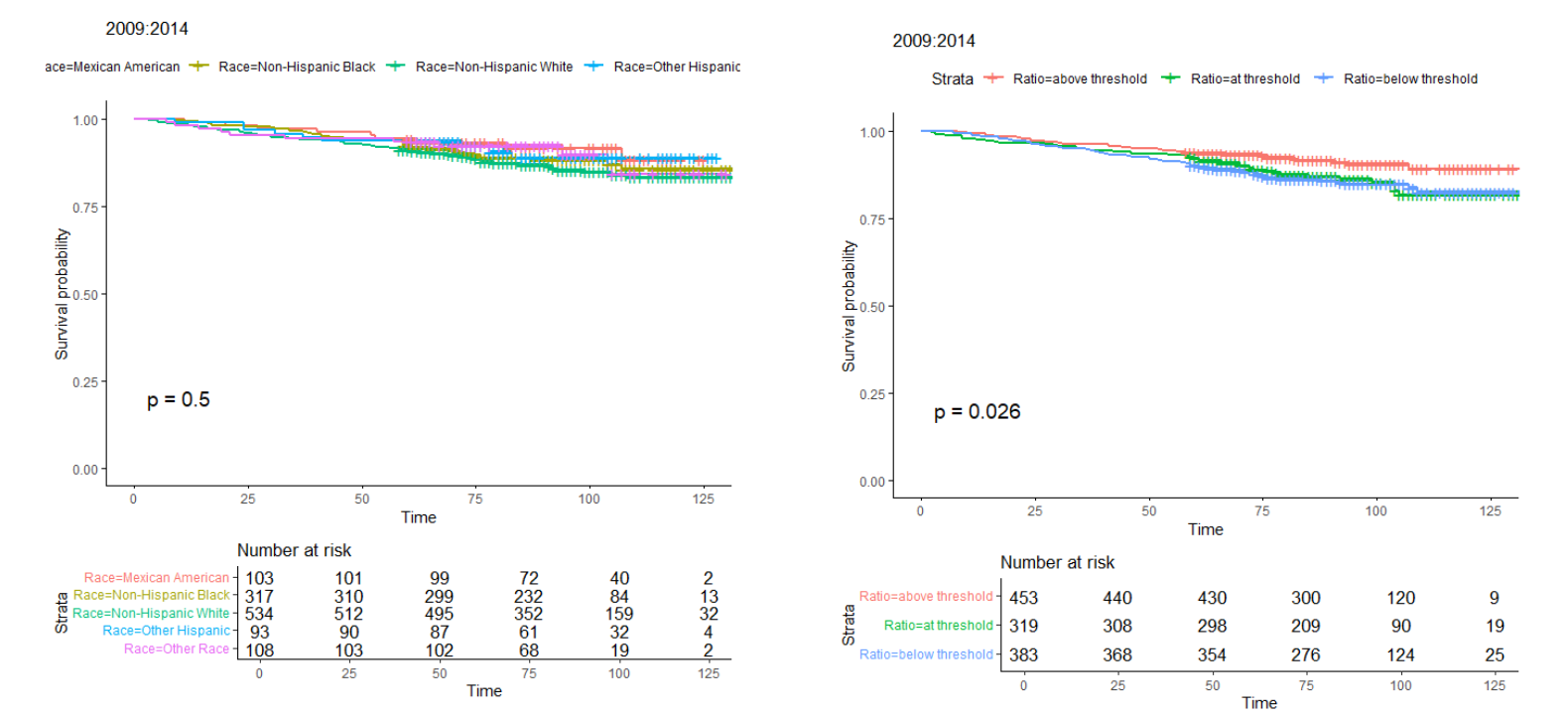
Results: In the pre-2015 period, Non-Hispanic Black participants had the lowest survival probabilities, reflecting the highest rates of emergency care visits. SES analyses revealed that participants below the income-to-poverty threshold also had significantly lower survival probabilities (p = 0.026). Post-2015, emergency care utilization decreased overall across racial and SES groups, with a modest improvement among Non-Hispanic Black participants. However, significant disparities persisted. Racial survival analyses post-2015 showed Non-Hispanic Black and Mexican American participants continued to have lower probabilities of avoiding emergency care compared to Non-Hispanic Whites, though differences were not statistically significant (p = 0.44). In SES analyses for 2015–2018, disparities became more pronounced. Participants below the income-to-poverty threshold remained disproportionately likely to use emergency care, with significantly lower survival probabilities compared to those above the threshold (p = 0.0037).
Conclusions: Although the introduction of biologic therapies post-2015 has contributed to an overall decline in emergency care visits for asthma, racial and socioeconomic disparities persist. Non-Hispanic Black and Mexican American participants, especially those with lower SES, remain disproportionately affected. These findings underscore the continued influence of SES on asthma-related outcomes, even after biologic therapies became available and highlight the need for targeted interventions to ensure equitable access to advanced asthma treatments and address socioeconomic barriers to care. Addressing these disparities is essential for reducing asthma-related healthcare utilization and improving outcomes in vulnerable populations.