Background: Urgency of and time to antibiotic administration has often been highlighted to prevent complications of community acquired pneumonia (CAP). Adult literature is mixed on whether administration of antibiotics within four hours of diagnosis of CAP reduces morbidity and mortality, however this has not been studied in pediatric patients. We evaluated whether time to antibiotics (within four hours of presentation to an Emergency Department (ED) versus greater than or equal to four hours) is associated with increased complications of CAP.
Methods: A multicenter, retrospective cohort study included children, three months to eighteen years, who had a CXR performed and were admitted from the ED for suspected CAP using data from the Pediatric Health Information System and manual chart review from 2013-2020. Bivariable analysis examined demographic and clinical characteristics between those that received antibiotics less than four hours from presentation versus greater than or equal to four hours from presentation. Inverse propensity weighted regression analyses were performed to assess the relationship of antibiotic receipt within four hours on primary and secondary outcomes. The primary outcome was a composite outcome of escalation of care. Secondary outcomes included length of stay, duration of oxygen use, cost of stay, seven-day pneumonia related ED revisits, and seven-day readmission rates.
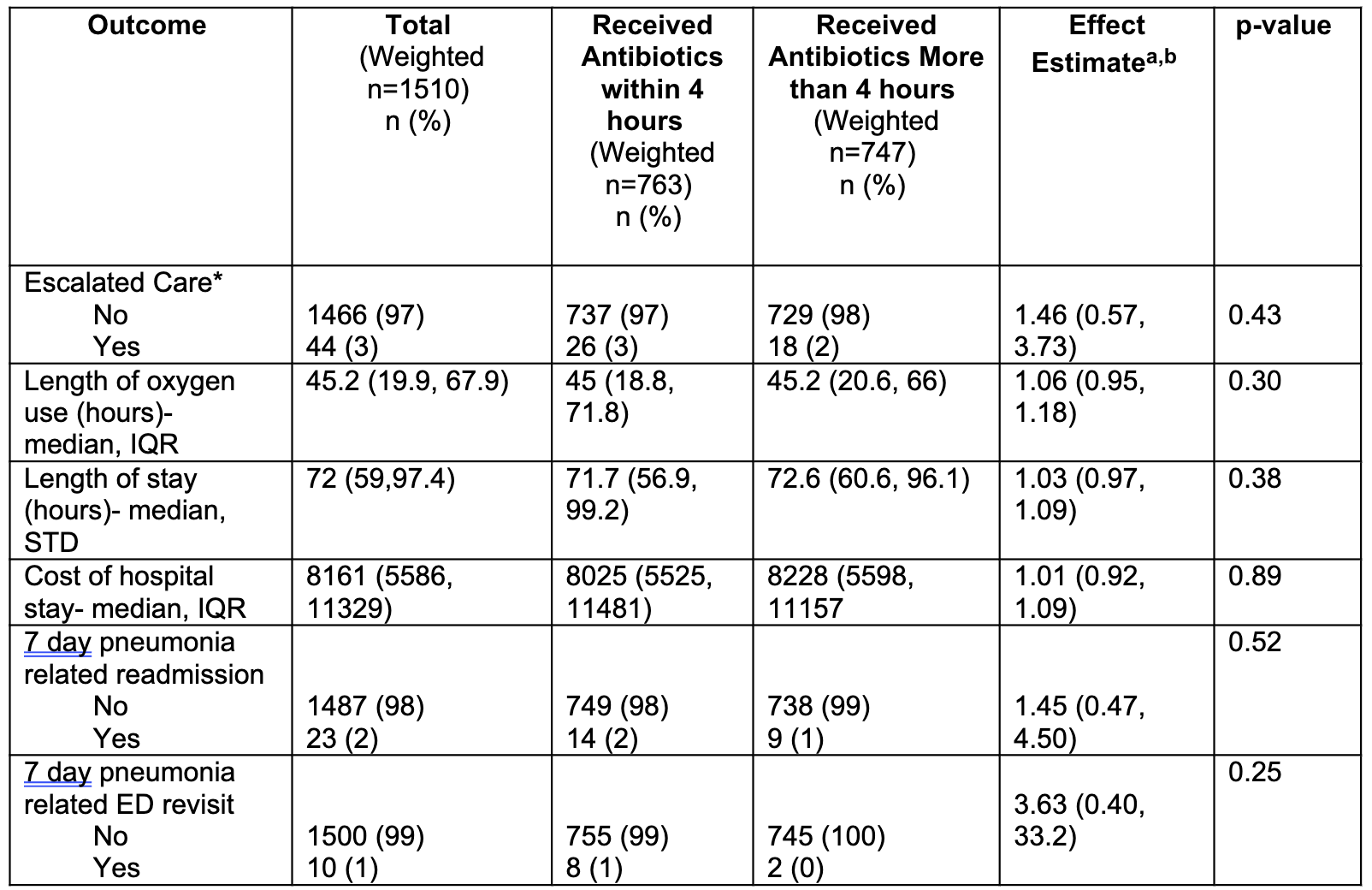
Results: Among 758 children hospitalized with CAP, 59% received an antibiotic within 4 hours from presentation. Patients who received antibiotics early were more likely to have crackles on exam and have hypoxemia in the ED (Table 1). In the inverse propensity weighted analyses, escalation of care occurred in 3% and 2% (p-value 0.4) of patients receiving antibiotics within 4 hours and greater than or equal to four hours, respectively, showing no difference in rates of complications. There was no difference in length of stay, duration of oxygen use, cost of stay, seven-day pneumonia related ED revisits, or seven- day readmission rates (Table 2).
Conclusions: Time to antibiotics did not change rates of escalation of care or the additional outcomes examined. These results vary from prior adult studies suggesting a different clinical course and microbiology of CAP in pediatric patients. According to these results, more time can be spent to confirm bacterial pneumonia to possibly limit antibiotic use and antibiotic morbidity. Further studies are needed to delineate which patients require antibiotics for improvement.